- Risk factors for breast cancer
-
Risk factors of breast cancer may be divided into preventable and non preventable. Their study belongs in the field of epidemiology. Breast cancer, like other forms of cancer, is considered to result from multiple environmental and hereditary risk factors.
Although many epidemiological risk factors have been identified, the cause of any individual breast cancer is most often unknowable. Epidemiological research informs the patterns of breast cancer incidence across certain populations, but not in a given individual. Approximately 5% of new breast cancers are attributable to hereditary syndromes and well-established risk factors accounted for approximately 30% of cases.[1]
Contents
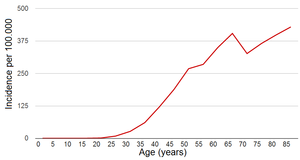
Age
The risk of getting breast cancer increases with age. A woman is more than 100 times more likely to develop breast cancer in her 60s than in her 20s.[3] If all women lived to age 95, about one in eight would be diagnosed with breast cancer at some point during their lives.[4] However, the actual lifetime risk is lower than that, because 90% of women die before age 95, most commonly from heart attacks, strokes, or other forms of cancer.
The probability of breast cancer rises with age, but breast cancer tends to be more aggressive in younger people.
Sex
Men have a much lower risk of developing breast cancer than women. In developed countries, about 99% of breast cancer cases are diagnosed in women; in a few African countries, which represent the highest incidence of male breast cancer, men account for 5–15% of breast cancer cases.[3] The rate of breast cancer in men appears to be rising somewhat.[5]
Men diagnosed with breast cancer tend to be older than women with breast cancer.[3] They are more likely to be diagnosed with hormone-receptor positive tumors, with about six out of seven cases being estrogen-receptor positive.[3] The overall prognosis is worse for men than for women.[3]
Heredity
Further information: Cancer syndrome and Hereditary breast-ovarian cancer syndromeUnited Kingdom being a member of the International Cancer Genome Consortium is leading efforts to map breast cancer's complete genome.
BRCA1 and BRCA2
In 5% of breast cancer cases, there is a strong inherited familial risk.[6]
Two autosomal dominant genes, BRCA1 and BRCA2, account for most of the cases of familial breast cancer. Women who carry a harmful BRCA mutation have a 60% to 80% risk of developing breast cancer in their lifetimes.[6] Other associated malignancies include ovarian cancer and pancreatic cancer. If a mother or a sister was diagnosed breast cancer, the risk of a hereditary BRCA1 or BRCA2 gene mutation is about 2-fold higher than those women without a familial history. Commercial testing for BRCA1 and BRCA2 gene mutations has been available in most developed countries since at least 2004.
In addition to the BRCA genes associated with breast cancer, the presence of NBR2, near breast cancer gene 1, has been discovered, and research into its contribution to breast cancer pathogenesis is ongoing.[7]
Other genes
Hereditary non-BRCA1 and non-BRCA2 breast tumors (and even some sporadic carcinomas) are believed to result from the expression of weakly penetrant but highly prevalent mutations in various genes. For instance, polymorphism has been identified in genes associated to the metabolism of estrogens and/or carcinogens (CYP1A1, CYP1B1, CYP17, CYP19, COMT, NAT2, GSTM1, GSTP1, GSTT, . . . ), to estrogen, androgen and vitamin D action (ESR1, AR, VDR), to co-activation of gene transcription (AIB1), to DNA damage response pathways (CHEK2, HRAS1, XRCC1, XRCC3, XRCC5).[8] Sequence variants of these genes that are relatively common in the population may be associated with a small to moderate increased relative risk for breast cancer. Combinations of such variants could lead to multiplicative effects. Sporadic cancers likely result from the complex interplay between the expression of low penetrance gene(s) (‘‘risk variants’’) and environmental factors. However, the suspected impact of most of these variants on breast cancer risk should, in most cases, be confirmed in large populations studies. Indeed, low penetrance genes cannot be easily tracked through families, as is true for dominant high-risk genes.[8]
Part of the hereditary non-BRCA1 and non-BRCA2 breast tumors may be associated to rare syndromes, of which breast cancer is only one component. Such syndromes result notably from mutations in TP53 (Li-Fraumeni syndrome), ATM (Ataxia Telangiectasia), STK11/LKB1(Peutz-Jeghers syndrome), PTEN (Cowden syndrome).
RAB11FIP1,[9] TP53, PTEN and rs4973768 are also associated with increased risk of breast cancer. rs6504950 is associated with lower risk of breast cancer.[10]
Mutations in RAD51C confer an increased risk for breast and ovarian cancer.[11]
Prior cancers
People who have previously been diagnosed with breast, ovarian, uterine, or bowel cancer have a higher risk of developing breast cancer in the future.[3] Mothers of children with soft-tissue sarcoma may have an increased risk of breast cancer.[3] Men with prostate cancer may have an elevated risk of breast cancer, although the absolute risk remains low.
Dietary factors
Alcohol
Main article: Alcohol and breast cancerAlcohol is a risk factor for breast cancer in women.[3][12]
A study of more than one million middle-aged British women concluded that each daily alcoholic beverage increases the incidence of breast cancer by 11 cases per 1000 women.[13] This means that among a group of 1000 women who have one drink per day, they will have 11 extra cases of breast cancer when compared to a group of women who drink less than one alcoholic beverage per week; a group of 1000 women who have four drinks per day will have an extra 44 cases of breast cancer compared to non-drinkers. One or two drinks each day increases the relative risk to 150% of normal, and six drinks per day increases the risk to 330% of normal. Approximately 6% of breast cancers reported in the UK are due to women drinking alcohol.[14]
The primary mechanism through which alcohol causes breast cancer is increased estrogen levels.[3]
Fat intake
Dietary influences have been examined since decades with conflicting results and so far failed to confirm any significant dependency. One recent study suggests that low-fat diets may significantly decrease the risk of breast cancer as well as the recurrence of breast cancer.[15] Another study showed no contribution of dietary fat intake on the incidence of breast cancer in over 300,000 women.[16] A randomized controlled study of the consequences of a low-fat diet, the Women's Health Initiative, failed to show a statistically significant reduction in breast cancer incidence in the group assigned to a low-fat diet, although the authors did find evidence of a benefit in the subgoup of women who followed the low-fat diet in a strict manner.[17] A prospective cohort study, the Nurses' Health Study II, found increased breast cancer incidence in premenopausal women only, with higher intake of animal fat, but not vegetable fat. Taken as a whole, these results point to a possible association between dietary fat intake and breast cancer incidence, though these interactions are hard to measure in large groups of women.
Specific dietary fatty acids
Although many claims have been made in popular literature there is no solid evidence linking specific fats to breast cancer.
A study published in 2001 found higher levels of monounsaturated fatty acids MUFAs (especially oleic acid) in the erythrocyte membranes of postmenopausal women who developed breast cancer.[18]
That same study discussed that a diet high in MUFAs is not the major determinant of erythrocyte membrane MUFAs, where most oleic acid in mammalian tissue is derived from the saturated stearic acid residue. Where key conversion is controlled by the Delta9-desaturase, which also regulates the transformation of the other common saturated fatty acids (SFAs) (myristic and palmitic). The study discussed that fat content of the diet has an important effect on Delta9-d activity, while high levels of SFAs increase Delta9-d activity by twofold to threefold, whereas polyunsaturated fatty acids (PUFAs) decrease.[18]
That conclusion was partially contradicted by a latter study, which showed a direct relation between very high consumption of omega-6 (PUFAs) and breast cancer in postmenopausal women.[19]
Phytoestrogens
Main article: Phytoestrogens#Health Risks and BenefitsPhytoestrogens have been extensively studied in animal and human in-vitro and epidemiological studies. Research failed to establish any noticeable benefit and some phytoestrogens may present a breast cancer risk.
The literature support the following conclusions:
- Plant estrogen intake in early adolescence may protect against breast cancer later in life.[20]
- The potential risks of isoflavones on breast tissue in women at high risk for breast cancer is still unclear.[21]
Vitamin D
Main article: Vitamin D#Role in cancer prevention and recoveryVitamin D is related to reduced risk of breast cancer and disease prognosis. A 2011 study done at the University of Rochester Medical Center found that low vitamin D levels among women with breast cancer correlate with more aggressive tumors and poorer prognosis. The study associated sub-optimal vitamin D levels with poor scores on every major biological marker that helps physicians predict a patient’s breast cancer outcome. The lead researcher stated, “Based on these results, doctors should strongly consider monitoring vitamin D levels among breast cancer patients and correcting them as needed.”[22]
Brassica vegetables
In a study published in the Journal of the American Medical Association, biomedical investigators found that Brassicas vegetable intake (broccoli, cauliflower, cabbage, kale and Brussels sprouts) was inversely related to breast cancer development. The relative risk among women in the highest decile of Brassica vegetable consumption (median, 1.5 servings per day) compared to the lowest decile (virtually no consumption) was 0.58. That is, women who consumed around 1.5 servings of Brassica vegetables per day had 42% less risk of developing breast cancer than those who consumed virtually none.[23]
Country diet
A significant environmental effect is likely responsible for the different rates of breast cancer incidence between countries with different dietary customs. Researchers have long measured that breast cancer rates in an immigrant population soon come to resemble the rates of the host country after a few generations. The reason for this is speculated to be immigrant uptake of the host country diet. The prototypical example of this phenomenon is the changing rate of breast cancer after the arrival of Japanese immigrants to America.[24]
Mushrooms
In 2009, a case-control study of the eating habits of 2,018 women suggested that women who consumed mushrooms had an approximately 50% lower incidence of breast cancer. Women who consumed mushrooms and green tea had a 90% lower incidence of breast cancer.[25] A case control study of 362 Korean women also reported an association between mushroom consumption and decreased risk of breast cancer.[26]
Iodine deficiency
The protective effects of iodine on breast cancer have been postulated from epidemiologic evidence and described in animal models.[27][28][29]
Obesity
Gaining weight after menopause can increase a woman's risk. A recent study found that putting on 9.9 kg (22 lbs) after menopause increased the risk of developing breast cancer by 18%.[30]
Hormones
Persistently increased blood levels of estrogen are associated with an increased risk of breast cancer, as are increased levels of the androgens androstenedione and testosterone (which can be directly converted by aromatase to the estrogens estrone and estradiol, respectively). Increased blood levels of progesterone are associated with a decreased risk of breast cancer in premenopausal women.[31] A number of circumstances which increase exposure to endogenous estrogens including not having children, delaying first childbirth, not breastfeeding, early menarche (the first menstrual period) and late menopause are suspected of increasing lifetime risk for developing breast cancer.[32]
However, not only sex hormones, but also insulin levels are positively associated with the risk of breast cancer.[33]
Pregnancy, childbearing and breastfeeding
Lower age of first childbirth, compared to the average age of 24,[34] having more children (about 7% lowered risk per child), and breastfeeding (4.3% per breastfeeding year, with an average relative risk around 0.7[35][36]) have all been correlated to lowered breast cancer risk in large studies.[37] Women who give birth and breast-feed by the age of 20 may have even greater protection.[38] In contrast, for instance, having the first live birth after age 30 doubles the risk compared to having first live birth at age less than 25.[39] Never having children triples the risk.[39]
Hormonal contraception
Hormonal contraceptives may produce a slight increase in the risk of breast cancer diagnosis among current and recent users, but this appears to be a short-term effect. In 1996 the largest collaborative reanalysis of individual data on over 150,000 women in 54 studies of breast cancer found a relative risk (RR) of 1.24 of breast cancer diagnosis among current combined oral contraceptive pill users; 10 or more years after stopping, no difference was seen. Further, the cancers diagnosed in women who had ever used hormonal contraceptives were less advanced than those in nonusers, raising the possibility that the small excess among users was due to increased detection.[40][41] The relative risk of breast cancer diagnosis associated with current and recent use of hormonal contraceptives did not appear to vary with family history of breast cancer.[42] Some studies have suggested that women who began using hormonal contraceptives before the age of 20 or before their first full-term pregnancy are at increased risk for breast cancer, but it is not clear how much of the risk stems from early age at first use, and how much stems from use before the first full-term pregnancy.[43]
Hormone replacement therapy
Data exist from both observational and randomized clinical trials regarding the association between menopausal hormone replacement therapy (menopausal HRT) and breast cancer. The largest meta-analysis (1997) of data from 51 observational studies, indicated a relative risk of breast cancer of 1.35 for women who had used HRT for 5 or more years after menopause.[citation needed] The estrogen-plus-progestin arm of the Women's Health Initiative (WHI), a randomized controlled trial, which randomized more than 16,000 postmenopausal women to receive combined hormone therapy or placebo, was halted early (2002) because health risks exceeded benefits. One of the adverse outcomes prompting closure was a significant increase in both total and invasive breast cancers (hazard ratio = 1.24) in women randomized to receive estrogen and progestin for an average of 5 years.[44] HRT-related breast cancers had adverse prognostic characteristics (more advanced stages and larger tumors) compared with cancers occurring in the placebo group, and HRT was also associated with a substantial increase in abnormal mammograms. Short-term use of hormones for treatment of menopausal symptoms appears to confer little or no breast cancer risk.[42] A correlation was found between the use of hormonal contraceptives and subsequent reliance on hormone replacement therapy.[43]
Oophorectomy and mastectomy
Main article: BRCA mutationProphylactic oophorectomy (removal of ovaries) and mastectomy in individuals with high-risk mutations of BRCA1 or BRCA2 genes reduces the risk of developing breast cancer as well as reducing the risk of developing ovarian cancer. Because of a complex balance of benefits and risks of a prophylactic surgery it is recommended only in very specific cases.
Hormonal therapy
Main article: Hormonal therapy (oncology)Hormonal therapy has been used for chemoprevention in individuals at high risk for breast cancer. Overall it is recommended only in very special circumstances. In 2002, a clinical practice guideline by the US Preventive Services Task Force (USPSTF) recommended that "clinicians discuss chemoprevention with women at high risk for breast cancer and at low risk for adverse effects of chemoprevention" with a grade B recommendation.[45][verification needed][46][47]
Selective estrogen receptor modulators (SERMs)
The guidelines[clarification needed] were based on studies of SERMs from the MORE, BCPT P-1, and Italian trials. In the MORE trial, the relative risk reduction for raloxifene was 76%.[48] The P-1 preventative study demonstrated that tamoxifen can prevent breast cancer in high-risk individuals. The relative risk reduction was up to 50% of new breast cancers, though the cancers prevented were more likely estrogen-receptor positive (this is analogous to the effect of finasteride on the prevention of prostate cancer, in which only low-grade prostate cancers were prevented).[49][50] The Italian trial showed benefit from tamoxifen.[51]
Additional randomized controlled trials have been published since the guidelines. The IBIS trial found benefit from tamoxifen.[52] In 2006, the NSABP STAR trial demonstrated that raloxifene had equal efficacy in preventing breast cancer compared with tamoxifen, but that there were fewer side effects with raloxifene.[53] The RUTH Trial concluded that "benefits of raloxifene in reducing the risks of invasive breast cancer and vertebral fracture should be weighed against the increased risks of venous thromboembolism and fatal stroke".[54] On September 14, 2007, the US Food and Drug Administration approved raloxifene (Evista) to prevent invasive breast cancer in postmenopausal women.[55]
Endocrine disruptors
Many xenoestrogens (industrially made estrogenic compounds) and other endocrine disruptors are potential risk factors of breast cancer.
Diethylstilbestrol (DES) is a synthetic form of estrogen. It has been used between the early 1940s and 1971. Pregnant women took DES to prevent certain pregnancy complications. However, it also increased their risk of breast cancer. It also increased the risk of breast cancer in the prenatally exposed daughters after they have reached an age 40 years.[56]
Furthermore, there is exposure to endocrine disruptors from the environment, in addition to phytoestrogens mentioned above in the diet section. See xenoestrogens in environmental factors below
Environmental factors
According to a review, the main mechanisms by which environmental compounds increase breast cancer risk are acting like hormones, especially estrogen, or affecting susceptibility to carcinogenesis.[57] The evidence to date generally supports an association between breast cancer and polycyclic aromatic hydrocarbons (PAHs) and polychlorinated biphenyls (PCBs). dioxins and organic solvents, on the other hand, have only shown an association in sparse and methodologically limited studies, but are suggestive of an association.[57] Overall, however, evidence is still based on a relatively small number of studies.[57]
Xenoestrogens
Many xenoestrogens (industrially made estrogenic compounds) are endocrine disruptors, and potential risk factors of breast cancer. Endocrine disruption is the hypothesis that some chemicals in the body, such as Bisphenol A, are capable of interfering with the production, processing, and transmission of hormones.[58]
A substantial and growing body of evidence indicates that exposures to certain toxic chemicals and hormone-mimicking compounds including chemicals used in pesticides, cosmetics and cleaning products contribute to the development of breast cancer.
The increasing prevalence of these substances in the environment may explain the increasing incidence of breast cancer, though direct evidence is sparse.
Bisphenol A
Bisphenol A (BPA) is a chemical compound used in the production of plastics found in numerous commercial products, including laptops, baby bottles, food containers, water main pipes, and laboratory and hospital equipment. BPA was first produced in 1891, but its estrogenic properties went undiscovered until the mid 1930s. Today it is considered a xenoestrogen, and it functions as an endocrine disruptor that interferes with hormones in the body and disrupts the normal functioning of the endocrine system. At very low levels the FDA has long considered BPA in food to be safe, but this has been challenged over the years as more information is discovered regarding the effects of the chemical.[59]
Rats exposed prenatally to environmentally relevant doses of BPA show an increased number of intraductal hyperplasias (precancerious lesions) in mammary glands that appear during adulthood, while high doses induce the development of carcinomas in breast tissue. Animals exposed to BPA during fetal life develop palpable tumors, and all studies show an increased susceptibility to mammary gland neoplasia that manifests during adulthood. Exposure of mouse dams to environmentally relevant levels of BPA during organogenesis results in considerable alterations in the mammary gland. It was concluded that perinatal exposure to low doses of BPA results in altered mammary gland morphogenesis, induction of precancerous lesions, and carcinoma in situ.[60]
A study sought to determine whether early exposure to BPA could accelerate mammary carcinogenesis in a dimethylbenzanthracene (DMBA) model of rodent mammary cancer. In the study, scientists exposed neonatal/prebubertal rats to BPA via lactation from nursing dams treated orally with 0, 25, and 250 µg BPA/kg body weight/day. For tumorigenesis studies, female offspring were exposed to 30 mg dimethylbenzanthracene (DMBA)/kg body weight at 50 days of age. DMBA induces mammary tumors and allows chemicals that predispose for mammary cancer to increase the number of mammary adenocarcinomas. The results of the study showed that female rats in the control, BPA 25, and BPA 250 groups administered DMBA exhibited a BPA dose-dependent increase in mammary tumors. The groups had 2.84, 3.82, and 5.00 mammary tumors per rat respectively. Treatment with BPA also reduced tumor latency, with the median tumor latency of 65, 53, and 56.5 days for 0, BPA 25, and BPA 250 groups respectively. Maternal exposure to BPA during lactation decreased time to first tumor latency and increased the number of DMBA-induced mammary tumors in female offspring. If these effects found in rodents carry over to humans, even minimal exposure to BPA could cause an increased risk for breast cancer.[61]
The elevated incidence of breast cancer in women has been associated with prolonged exposure to high levels of estrogens. Xenoestrogens, such as BPA have the capacity to perturb normal hormonal actions. This study provides evidence of the estrogenic effects of BPA. In this study the human breast epithelial cells MCF-10F were treated with 10-3 M, 10-4 M, 10-5 M and 10-6 M BPA continuously for two weeks. The cells treated with 10-3 M BPA died on the second day of treatment. The concentration of 10-4 M BPA was also toxic for the breast epithelial cells, and they died on the fourth day of treatment. This data indicated that these concentrations of BPA are toxic for MCF-10F cells. After the two-week observation period it was seen that the cells formed a high percentage of duct like structures in collagen. MCF-10F cells treated with 10-5 M and 10-6 M BPA formed a high percentage of solid masses, 27% and 20% respectively. This data indicates that BPA is able to induce neoplastic transformation of human breast epithelial cells. Epigenetic changes are involved in the early stages of cancer initiation by altering ductulogenesis. BPA was able to induce transformation of human breast MCF-10F epithelial cells. After treatment with BPA, the cells produced fewer collagen tubules and more solid masses.[62]
Consumer groups recommend that people wishing to lower their exposure to bisphenol A avoid canned food and polycarbonate plastic containers (which shares resin identification code 7 with many other plastics) unless the packaging indicates the plastic is bisphenol A-free.[63] The National Toxicology Panel recommends avoiding microwaving food in plastic containers, putting plastics in the dishwasher, or using harsh detergents on plastics, to avoid leaching.[64]
Aromatic Amines
Aromatic amines are chemicals that are produced when products such as dyes, polyurethane products, and certain pesticides are made. They are also found in cigarette smoke, fuel exhaust, and in over cooked, burned meat. The three types of aromatic amines monocyclic, polycyclic, and heterocyclic have all been found in recent studies of breast health. Monocyclic amines have been found to cause mammary cancer in rats. Studies have shown that women who eat higher amounts of overcooked meat, meaning more exposure to heterocyclic amines, have also been diagnosed with more post-menopausal breast cancer. Heterocyclic amines also have the ability to copy estrogen and in laboratory studies have been found to encourage the growth of cancerous tumors on human tissue.[65]
Benzene
Benzene is a petrochemical solvent. Benzene exposure mostly originates from air pollution resulting from industrial burning, exhaust and gas fumes, as well as cigarette smoke. The International Agency for Research on Cancer and the National Toxicology Program have labeled benzene as a definite human carcinogen. Multiple studies point to a correlation between benzene exposure and breast cancer risk. Laboratory studies on mice have shown that a high level of benzene exposure can lead to mammary cancer.[65]
DDT
Main article: DDT#Breast cancerAlthough the pesticide DDT was banned over 20 years ago, studies have shown that there are still trace amounts found in certain agricultural products, as well as in human and animal milk.[66] While individual studies have come to conflicting conclusions, the most recent reviews of all the evidence conclude that exposure to DDT before puberty increases the risk of breast cancer later in life.[67][68]
Ethylene oxide
Ethylene oxide is a chemical that can be found in some personal care products, mainly in the form of fragrance. It is also used for the sterilization of various medical objects. The National Toxicology Program has labeled ethylene oxide as a definite human and animal carcinogen. A study done by the National Institute for Occupational Safety and Health including 7,576 women found a direct correlation between breast cancer rates and exposure to ethylene oxide during medical sterilization processes. Also, human breast cells put into contact with small amounts of ethylene oxide in a laboratory can lead to DNA damage of the breast tissue.[65]
Polycyclic aromatic hydrocarbons
Polycyclic aromatic hydrocarbons are chemical products of combustion from coal burners, fuel, cigarette smoke, and various other sources. PAH's are often found in the air and are breathed into the body. PAH's bioaccumulate easily and can copy the estrogen hormone. PAH's can also be genotoxic, meaning they have the ability to harm DNA.[65]
Vinyl chloride
Vinyl chloride is produced when PVC or polyvinly chloride is made. PVC is found in plastic packaging, outerwear, plastic toys and other plastic products. Vinyl chloride can be found in cigarette smoke and the air around garbage and land fills. It can also be found in the wastewater when PVC is made. The National Toxicology Program and the International Agency for Research on Cancer have both labeled vinyl chloride as a definite human carcinogen.[65]
Tobacco
Until recently, most studies had not found an increased risk of breast cancer from active tobacco smoking. Beginning in the mid-1990s, a number of studies suggested an increased risk of breast cancer in both active smokers and those exposed to secondhand smoke compared to women who reported no exposure to secondhand smoke.[69] By 2005 enough evidence had accumulated for the [California Environmental Protection Agency] to conclude that breathing secondhand smoke causes breast cancer in younger, primarily premenopausal women.[70] The Agency concluded that the risk was increased by 70%, based on epidemiological studies and the fact that there are many mammary carcinogens in secondhand smoke. The following year (2006) the US Surgeon General[71] identified the same risk increase and concluded that the evidence is "suggestive," one step below causal. There is some evidence that exposure to tobacco smoke is most problematic between puberty and first childbirth. The reason is that breast tissue appears most sensitive to chemical carcinogens breast cells not fully differentiated until lactation.[72] The likely reason that the older studies of active smoking did not detect risks associated with smoking was that they compared active smokers to all nonsmokers (which includes many passive smokers). The newer studies, which exclude passive smokers from the control group, generally show elevated risks associated with active as well as passive smoking.
Passive smoking
Breathing secondhand smoke increases breast cancer risk by 70% in younger, primarily pre-menopausal women. The California Environmental Protection Agency has concluded that passive smoking causes breast cancer[70] and the US Surgeon General[71] has concluded that the evidence is "suggestive," one step below causal. There is some evidence that exposure to tobacco smoke is most problematic between puberty and first childbirth. The reason that breast tissue appears most sensitive to chemical carcinogens in this phase is that breast cells are not fully differentiated until lactation.[72]
Radiation
Women who have received high-dose ionizing radiation to the chest (for example, as treatments for other cancers) have a relative risk of breast cancer between 2.1 to 4.0.[69] The risk increases with increased dose. In addition, the risk is higher in women irradiated before age 30, when there is still breast development.[39]
Dioxins
Dioxins (most notably the polychlorinated dibenzodioxins) are chemicals that are produced when chlorinated products are burned, such as polyvinyl chloride (PVC). This occurs when chlorinated products are used in certain manufacturing industries. Dioxins are also added to the air when gasoline and diesel fuels break down. Dioxins are able to bioaccumulate, meaning that they settle and stay in human and animal fat for long periods of time. There are many different types of dioxins and only a few of them have been labeled by the Environmental Protection Agency as definite human carcinogens and endocrine hormone disruptors. Although dioxins are floating in the air, they eventually settle on plants and other vegetation surfaces. These plants and vegetation are them eaten by cows and other animals. Humans end up eating the produce, milk, eggs, and meat produced by these animals that have consumed dioxin covered vegetation. Dioxins are more harmful when ingested this way. Multiple studies have led to the idea that increased dioxin levels can increase one's risk for breast cancer. A study done in 1976 after a chemical plant explosion in Seveso, Italy concluded that high dioxin level exposure in a woman's body correlated with a more than double chance of developing breast cancer.[65]
Light at night and disturbance of circadian rhythm
In 1978 Cohen et al. proposed that reduced production of the hormone melatonin might increase the risk of breast cancer and citing "environmental lighting" as a possible causal factor.[73] Researchers at the National Cancer Institute (NCI) and National Institute of Environmental Health Sciences conducted a study in 2005 that suggests that artificial light during the night can be a factor for breast cancer by disrupting melatonin levels.[74]
In 2007, "shiftwork that involves circadian disruption" was listed as a probable carcinogen by the World Health Organization's International Agency for Research on Cancer. (IARC Press release No. 180).[75] Multiple studies have documented a link between night shift work and the increased incidence of breast cancer.[76][77][78][79] A review of current knowledge of the health consequences of exposure to artificial light at night including the increased incidence of breast cancer and an explanation of the causal mechanisms has been published in the Journal of Pineal Research in 2007.[80]
Racial and socioeconomic factors
Incidence and mortality vary with race and social status. Incidence rises with improving economic situation, while mortality is tied to low economic status. In the US incidence is significantly lower and mortality higher among black women and this difference appears to persist even after adjustment for economic status. It is currently unclear if significant racial differences in incidence and mortality persist after adjustment for economic status between women of white, Hispanic and asian origin in the US.[81]
Several studies have found that black women in the U.S. are more likely to die from breast cancer even though white women are more likely to be diagnosed with the disease. Even after diagnosis, black women are less likely to get treatment compared to white women.[82][83][84] Scholars have advanced several theories for the disparities, including inadequate access to screening, reduced availability of the most advanced surgical and medical techniques, or some biological characteristic of the disease in the African American population.[85] Some studies suggest that the racial disparity in breast cancer outcomes may reflect cultural biases more than biological disease differences.[86] However, the lack of diversity in clinical trials for breast cancer treatment may contribute to these disparities, with recent research indicating that black women are more likely to have estrogen receptor negative breast cancers, which are not responsive to hormone treatments that are effective for most white women.[87] Research is currently ongoing to define the contribution of both biological and cultural factors.[83][88]
Part of the differences in incidence that is attributable to race and economic status may be explained by past use of hormone replacement therapy[89]
Factors with inconclusive research
Tea
One research published in 2009 has show that moderate green or black tea consumption (three or more cups per day) can reduce breast cancer risk by 37% in women younger than 50 years old, comparing with women who drank no tea at all. But no association was found for overall women.[90] However that study has been criticized for inaccuracy[91] and another study found no substantial association between and tea consumption in the overall, but found a weak inverse association between caffeine-containing beverages and risk of postmenopausal breast cancer.[92]
Specifically about green tea, one study has found significant inverse association between risk of breast cancer and green tea intake in Asian women who were low soy consumers.[93]
1,3-Butadiene
1,3-Butadiene is an environmental factor that can be found in air pollution and can be produced by combustion engines, as well as petroleum refineries. It is found in cigarette smoke and is also used in the making and processing of certain synthetic rubber products and fungicides. The National Toxicology Program has labeled 1,3-Butadiene as definite human carcinogen. The EPA has stated that people are mainly put in contact with this chemical through the means of simple inhalation.[65]
Mammographic density
Mammographic density refers to the relative proportions of radiodense area compared to the radiolucent area on a mammogram, which is basically an x-ray of the breast. The radiodense area on a mammogram is white and is associated with ductal and lobular epithelium, connective tissue and fluid in the breast. The radiolucent area is dark gray or black and is associated with fat in the breast. High mammographic density is associated with a higher risk of developing breast cancer, but the reasons for this link are not certain and are being studied.[94][95]
Red No. 3
Red No. 3 is a coloring agent used in some foods. In laboratory tests human breast cell DNA was found positive for damage when put into contact with Red No. 3, which means that it is genotoxic.[96]
Factors with minimal or no impact
Abortion
Main article: Abortion – breast cancer hypothesisThe abortion-breast cancer (ABC) hypothesis (supporters call it the abortion-breast cancer link) posits induced abortion increases the risk of developing breast cancer;[97] it is a controversial subject and the current scientific consensus has concluded there is no significant association between first-trimester abortion and breast cancer risk.[98][99]
Bras
There is no scientific evidence to prove that any kind of bra can cause cancer.[100]
Deodorants
Much has been made of the possible contribution of aluminum-containing underarm antiperspirants to the incidence of breast cancer, since the most common location of a breast cancer is the upper outer quadrant of the breast. Aluminum salts, such as those used in anti-perspirants, have recently been classified as metalloestrogens. In research published in the Journal of Applied Toxicology, Dr. Philippa D. Darbre of the University of Reading has shown that aluminum salts increase estrogen-related gene expression in human breast cancer cells grown in the laboratory.[101][102][103] Fortunately, this in-vitro association between aluminum salts and estrogen activity does not translate into an increased risk of breast cancer in humans. The lack of association between underarm deodorants and breast cancer has been the subject of a number of research articles.[104][105]
Fertility treatments
There is no persuasive connection between fertility medications and breast cancer.[106]
Folic acid (folate)
Main article: Folic acid#CancerThe results of the studies about the influence of dietary folic acid on breast cancer have been contradictory.
Viruses
Several kind of viruses are suspected to play a role or cause breast cancer, among them human papilloma virus[107], human cytomegalovirus[108] and the Epstein-Barr virus[109]. The human papilloma virus is well known for its capability to immortalize breast cancer cells which is used in research, however the role of this viruses in human breast cancer remains controversial.
Humans are not the only mammals susceptible to breast cancer. Some strains of mice, namely the house mouse (Mus domesticus) are prone to breast cancer which is caused by infection with the mouse mammary tumour virus (MMTV or "Bittner virus" for its discoverer Hans Bittner), by random insertional mutagenesis. This finding is taken to mean that a viral origin of human breast cancer is at least possible, though there is no definitive evidence to support the claim that MMTV causes human breast cancer. For example, there may be critical differences between cancer pathogenesis in mice and people. A human homologue of the mammary virus has been described in 1971 and linked to to human breast cancer in several small epidemiologic studies.[110][111]
History
In past centuries, the development of breast cancer was most commonly seen as divine punishment or a trial. From ancient Greek medicine until the end of the 17th century, the dominant medical explanation was an imbalance of the four humors.[112] By the start of the 18th century, humoralism had generally been rejected. Many other theories were put forward, often related to sexual activity: In 1713, Bernardino Ramazzini said that nuns developed breast cancer at a higher rate than married women because they did not engage in sexual intercourse, and the "unnatural" lack of sexual activity caused instability of the breasts; others countered that the cause was frequently too much sexual activity.[113] Other theories from the 18th century included various sorts of problems with the movement of body fluids, such as lymphatic blockages, curdled breast milk or the transformation of pus left after an infection.[113]
In modern times, women are more likely to blame themselves, perhaps deciding that their diet, childbearing history, decision not to breastfeed, or level of exercise is the cause.[112]
References
- ^ Madigan MP, Ziegler RG, Benichou J, Byrne C, Hoover RN (1995). "Proportion of breast cancer cases in the United States explained by well-established risk factors". J. Natl. Cancer Inst. 87 (22): 1681–5. doi:10.1093/jnci/87.22.1681. PMID 7473816.
- ^ Excel chart for Figure 1.1: Breast Cancer (C50), Average Number of New Cases per Year and Age-Specific Incidence Rates, UK, 2006-2008 at Breast cancer - UK incidence statistics at Cancer Research UK. Section updated 18/07/11.
- ^ a b c d e f g h i Margolese, Richard G, Bernard Fisher, Gabriel N Hortobagyi, and William D Bloomer (2000). "118". In Bast RC, Kufe DW, Pollock RE, et al.. Cancer Medicine (e.5 ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20900/#A29677. Retrieved 27 January 2011.
- ^ Olson, James Stuart (2002). Bathsheba's Breast: Women, Cancer and History. Baltimore: The Johns Hopkins University Press. pp. 199–200. ISBN 0-8018-6936-6. OCLC 186453370.
- ^ Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN (July 2004). "Breast carcinoma in men: a population-based study". Cancer 101 (1): 51–7. doi:10.1002/cncr.20312. PMID 15221988.
- ^ a b Malone KE, Daling JR, Thompson JD, O'Brien CA, Francisco LV, Ostrander EA (1998). "BRCA1 mutations and breast cancer in the general population: analyses in women before age 35 years and in women before age 45 years with first-degree family history". JAMA 279 (12): 922–9. doi:10.1001/jama.279.12.922. PMID 9544766.
- ^ Emilie Auriol, Lise-Marie Billard, Frederique Magdinier, Robert Dante (2005). "Specific binding of the methyl binding domain protein 2 at the BRCA1-NBR2 locus". Nucleic Acids Research 33 (13): 4243–4254. doi:10.1093/nar/gki729. PMC 1181861. PMID 16052033. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1181861.
- ^ a b Lacroix, M; Leclercq, G. (2005). "The "portrait" of hereditary breast cancer". Breast Cancer Research and Treatment 89 (3): 297–304. doi:10.1007/s10549-004-2172-4. PMID 15754129.
- ^ Zhang, J.; Liu, X.; Datta, A.; Govindarajan, K.; Tam, L.; Han, J.; George, J.; Wong, C. et al. (Jul 2009). "RCP is a human breast cancer-promoting gene with Ras-activating function" (Free full text). The Journal of clinical investigation 119 (8): 2171–2183. doi:10.1172/JCI37622. ISSN 0021-9738. PMC 2719918. PMID 19620787. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2719918.
- ^ "Breast cancer gene 'could reduce risk'". The Daily Telegraph (London). 2009-03-30. http://www.telegraph.co.uk/health/healthnews/5071129/Breast-cancer-gene-could-reduce-risk.html. Retrieved 2010-05-22.
- ^ Meindl A, Hellebrand H, Wiek C, et al. (May 2010). "Germline mutations in breast and ovarian cancer pedigrees establish RAD51C as a human cancer susceptibility gene". Nature Genetics 42 (5): 410–4. doi:10.1038/ng.569. PMID 20400964.
- ^ Room, R; Babor, T; Rehm, J (2005). "Alcohol and public health". The Lancet 365 (9458): 519–30. doi:10.1016/S0140-6736(05)17870-2. PMID 15705462.
- ^ Allen NE, Beral V, Casabonne D, et al. (March 2009). "Moderate alcohol intake and cancer incidence in women". Journal of the National Cancer Institute 101 (5): 296–305. doi:10.1093/jnci/djn514. PMID 19244173.
- ^ Non-Technical Summary Committee on Carcinogenicity of Chemicals in Food Consumer Products and the Environment (COC)
- ^ Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, et al. (2006). "Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study (WINS)". J Natl Cancer Inst 98 (24): 1767–1776. doi:10.1093/jnci/djj494. PMID 17179478.
- ^ Hunter DJ, Spiegelman D, Adami HO, et al. (1996). "Cohort studies of fat intake and the risk of breast cancer--a pooled analysis". N. Engl. J. Med. 334 (6): 356–61. doi:10.1056/NEJM199602083340603. PMID 8538706.
- ^ Prentice RL, Caan B, Chlebowski RT, et al. (2006). "Low-fat dietary pattern and risk of invasive breast cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial". JAMA 295 (6): 629–42. doi:10.1001/jama.295.6.629. PMID 16467232.
- ^ a b Pala V, Krogh V, Muti P, et al. (July 2001). "Erythrocyte membrane fatty acids and subsequent breast cancer: a prospective Italian study". Journal of the National Cancer Institute 93 (14): 1088–95. doi:10.1093/jnci/93.14.1088. PMID 11459870.
- ^ Sonestedt, Emily; Ericson, Ulrika; Gullberg, Bo; Skog, Kerstin; Olsson, Håkan; Wirf�lt, Elisabet (2008). "Do both heterocyclic amines and omega-6 polyunsaturated fatty acids contribute to the incidence of breast cancer in postmenopausal women of the Malmö diet and cancer cohort?". International Journal of Cancer 123 (5482): 1637. doi:10.1002/ijc.23394. PMID 10970215.
- ^ Rice S, Whitehead SA (2006). "Phytoestrogens and breast cancer--promoters or protectors?". Endocr. Relat. Cancer 13 (4): 995–1015. doi:10.1677/erc.1.01159. PMID 17158751.
- ^ Messina M, McCaskill-Stevens W, Lampe JW (September 2006). "Addressing the soy and breast cancer relationship: review, commentary, and workshop proceedings". Journal of the National Cancer Institute 98 (18): 1275–84. doi:10.1093/jnci/djj356. PMID 16985246.
- ^ http://www.urmc.rochester.edu/news/story/index.cfm?id=3182
- ^ Terry P, Wolk A, Persson I, Magnusson C (2001). "Brassica Vegetables and Breast Cancer Risk". JAMA the Journal of the American Medical Association 285 (23): 2975–2976. doi:10.1001/jama.285.23.2975. PMID 11410091.
- ^ Nelson N (2006). "Migrant Studies Aid Search for Factors Linked to Breast Cancer Risk". JAMA 8 (7): 436–438.
- ^ Zhang, M; Huang, J; Xie, X; Holman, CD (2009). "Dietary intakes of mushrooms and green tea combine to reduce the risk of breast cancer in Chinese women.". International Journal of Cancer (International Journal of Cancer (Online)) 124 (6): 1404–1408. doi:10.1002/ijc.24047. PMID 19048616
- ^ Hong, SA; Kim, K; Nam, SJ; Kong, G; Kim, MK (2008). "A case-control study on the dietary intake of mushrooms and breast cancer risk among Korean women.". International journal of cancer. Journal international du cancer 122 (4): 919–23. doi:10.1002/ijc.23134. PMID 17943725
- ^ Venturi, S. (2001). "Is there a role for iodine in breast diseases?". The Breast 10 (5): 379–382. doi:10.1054/brst.2000.0267. PMID 14965610.
- ^ Aceves, C.; Anguiano, B.; Delgado, G. (2005). "Is iodine a gatekeeper of the integrity of the mammary gland?". Journal of mammary gland biology and neoplasia 10 (2): 189–196. doi:10.1007/s10911-005-5401-5. PMID 16025225.
- ^ Stoddard Fr, 2nd; Brooks, AD; Eskin, BA; Johannes, GJ (2008). "Iodine alters gene expression in the MCF7 breast cancer cell line: evidence for an anti-estrogen effect of iodine". International journal of medical sciences 5 (4): 189–96. PMC 2452979. PMID 18645607. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2452979.
- ^ BBC report Weight link to breast cancer risk
- ^ Yager JD; Davidson NE (2006). "Estrogen carcinogenesis in breast cancer". New Engl J Med 354 (3): 270–82. doi:10.1056/NEJMra050776. PMID 16421368.
- ^ American Cancer Society. (2006-10-03). What Are the Risk Factors for Breast Cancer? Retrieved 2006-03-30.
- ^ http://jnci.oxfordjournals.org/cgi/content/abstract/101/1/48
- ^ http://www.medscape.com/viewarticle/517532
- ^ McTiernan A, Thomas DB (September 1986). "Evidence for a protective effect of lactation on risk of breast cancer in young women. Results from a case-control study". Am. J. Epidemiol. 124 (3): 353–8. PMID 3740036. http://aje.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=3740036.
- ^ Byers T, Graham S, Rzepka T, Marshall J (May 1985). "Lactation and breast cancer. Evidence for a negative association in premenopausal women". American Journal of Epidemiology 121 (5): 664–74. doi:10.1093/aje/121.5.664. PMID 4014158.
- ^ "Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer". Lancet 350 (9084): 1047–59. 1997. doi:10.1016/S0140-6736(97)08233-0. PMID 10213546. http://linkinghub.elsevier.com/retrieve/pii/S0140673697082330. Retrieved 2008-04-08.
- ^ Newcomb PA, Storer BE, Longnecker MP, Mittendorf R, Greenberg ER, Clapp RW, Burke KP, Willett WC, MacMahon B. (1994-01-13). "Lactation and a reduced risk of premenopausal breast cancer". New England Journal of Medicine 330 (2): 81–7. doi:10.1056/NEJM199401133300201. PMID 8259187.
- ^ a b c Chapter 19 in: Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson. Robbins Basic Pathology. Philadelphia: Saunders. ISBN 1-4160-2973-7. 8th edition
- ^ Collaborative Group on Hormonal Factors in Breast Cancer (1996). "Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53,297 women with breast cancer and 100,239 women without breast cancer from 54 epidemiological studies". Lancet 347 (9017): 1713–27. doi:10.1016/S0140-6736(96)90806-5. PMID 8656904.
- ^ Collaborative Group on Hormonal Factors in Breast Cancer (1996). "Breast cancer and hormonal contraceptives: further results". Contraception 54 (3 Suppl): 1S–106S. doi:10.1016/0010-7824(96)00111-4. PMID 8899264.
- ^ a b National Cancer Institute (2006-08-03). "Hormone Therapy". Genetics of Breast and Ovarian Cancer. http://www.cancer.gov/cancertopics/pdq/genetics/breast-and-ovarian/healthprofessional#Section_340. Retrieved 2006-08-12.
- ^ a b World Health Organization International Agency for Research on Cancer (1999). "Hormonal Contraception and Post-menopausal Hormonal Therapy". IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. http://monographs.iarc.fr/ENG/Monographs/vol72/mono72.pdf. Retrieved 12 March 2011.
- ^ Heiss, G.; Wallace, R.; Anderson, G. L.; Aragaki, A.; Beresford, S. A. A.; Brzyski, R.; Chlebowski, R. T.; Gass, M. et al. (2008). "Health Risks and Benefits 3 Years After Stopping Randomized Treatment with Estrogen and Progestin". JAMA: the Journal of the American Medical Association 299 (9): 1036. doi:10.1001/jama.299.9.1036.
- ^ "Guide to Clinical Preventive Services, Third Edition: Periodic Updates, 2000–2003". Agency for Healthcare Research and Quality. US Preventive Services Task Force. http://www.ahrq.gov/clinic/3rduspstf/ratings.htm. Retrieved 2007-10-07.
- ^ U.S. Preventive Services Task Force (2002). "Chemoprevention of breast cancer: recommendations and rationale". Ann. Intern. Med. 137 (1): 56–8. PMID 12093249. http://www.annals.org/cgi/content/full/137/1/56.
- ^ Kinsinger LS, Harris R, Woolf SH, Sox HC, Lohr KN (2002). "Chemoprevention of breast cancer: a summary of the evidence for the U.S. Preventive Services Task Force". Ann. Intern. Med. 137 (1): 59–69. PMID 12093250. http://www.annals.org/cgi/content/full/137/1/59.
- ^ Cummings SR, Eckert S, Krueger KA, et al. (1999). "The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation". JAMA 281 (23): 2189–97. doi:10.1001/jama.281.23.2189. PMID 10376571.
- ^ Fisher B, Costantino JP, Wickerham DL, et al. (2005). "Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study". J. Natl. Cancer Inst. 97 (22): 1652–62. doi:10.1093/jnci/dji372. PMID 16288118.
- ^ Fisher B, Costantino JP, Wickerham DL, et al. (1998). "Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study". J. Natl. Cancer Inst. 90 (18): 1371–88. doi:10.1093/jnci/90.18.1371. PMID 9747868.
- ^ Veronesi U, Maisonneuve P, Rotmensz N, et al. (2007). "Tamoxifen for the prevention of breast cancer: late results of the Italian Randomized Tamoxifen Prevention Trial among women with hysterectomy". J. Natl. Cancer Inst. 99 (9): 727–37. doi:10.1093/jnci/djk154. PMID 17470740.
- ^ Cuzick J, Forbes JF, Sestak I, et al. (2007). "Long-term results of tamoxifen prophylaxis for breast cancer--96-month follow-up of the randomized IBIS-I trial". J. Natl. Cancer Inst. 99 (4): 272–82. doi:10.1093/jnci/djk049. PMID 17312304.
- ^ Vogel VG, Costantino JP, Wickerham DL, et al. (2006). "Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial". JAMA 295 (23): 2727–41. doi:10.1001/jama.295.23.joc60074. PMID 16754727.
- ^ Barrett-Connor E, Mosca L, Collins P, et al. Raloxifene Use for The Heart (RUTH) Trial Investigators. (2006). "Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women". N. Engl. J. Med. 355 (2): 125–37. doi:10.1056/NEJMoa062462. PMID 16837676.
- ^ AFP.google.com, US approves Lilly's Evista for breast cancer prevention
- ^ Palmer JR, Wise LA, Hatch EE, et al. (August 2006). "Prenatal diethylstilbestrol exposure and risk of breast cancer". Cancer Epidemiology, Biomarkers & Prevention 15 (8): 1509–14. doi:10.1158/1055-9965.EPI-06-0109. PMID 16896041.
- ^ a b c Brody JG, Moysich KB, Humblet O, Attfield KR, Beehler GP, Rudel RA (June 2007). "Environmental pollutants and breast cancer: epidemiologic studies". Cancer 109 (12 Suppl): 2667–711. doi:10.1002/cncr.22655. PMID 17503436.
- ^ Vogel SA (November 2009). "The Politics of Plastics: The Making and Unmaking of Bisphenol A Safety". American Journal of Public Health 99 (S3): 559–66. doi:10.2105/AJPH.2008.159228. PMID 19890158.
- ^ Vogel SA (2009). "The Politics of Plastics: The Making and Unmaking of Bisphenol A Safety". American Journal of Public Health 99 (3): 559–66. doi:10.2105/AJPH.2008.159228. PMID 19890158.
- ^ Soto AM, Sonnenschein C (2010). "Environmental Causes of Cancer: Endocrine Disruptors as Carcinogens". Nature Reviews Endocrinology 6 (7): 363–70. doi:10.1038/nrendo.2010.87. PMID 20498677.
- ^ Jenkins S, Raghuraman N, Eltoum I, Carpenter M, Russo J, Lamartiniere CA (2009). "Oral Exposed to Bisphenol A Increases DMBA-Induced Mammary Cancer in Rats". Environmental Health Perspectives 117: 910–17. doi:10.1289/ehp.11751. PMC 2702405. PMID 19590682. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2702405.
- ^ Fernandez SV, Russo J (2010). "Estrogens and Xenoestrogens in Breast Cancer". Toxicologic Pathology 38 (1): 110–22. doi:10.1177/0192623309354108. PMC 2907875. PMID 19933552. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2907875.
- ^ http://www.loe.org/shows/segments.htm?programID=08-P13-00038&segmentID=4
- ^ FDA Weighs Safety Of Bisphenol A
- ^ a b c d e f g State of the Evidence, The Connection Between Breast Cancer and the Environment, 2008
- ^ Chemical Contaminants in Human Milk: An Overview. Babasaheb R. Sonawane. Environmental Health Perspectives, Vol.103, pp.197–205.
- ^ Eskenazi, Brenda; Jonathan Chevrier, Lisa Goldman Rosas, Henry A. Anderson, Maria S. Bornman, Henk Bouwman, Aimin Chen, Barbara A. Cohn, Christiaan de Jager, et al. (May 4, 2009). "The Pine River Statement: Human Health Consequences of DDT Use". Environmental Health Perspectives Online ahead of print. http://www.ehponline.org/members/2009/11748/11748.pdf.
- ^ Clapp RW, Jacobs MM, Loechler EL (2008). "Environmental and occupational causes of cancer: new evidence 2005-2007". Reviews on Environmental Health 23 (1): 1–37. PMC 2791455. PMID 18557596. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2791455.
- ^ a b ACS (2005). "Breast Cancer Facts & Figures 2005–2006" (PDF). Archived from the original on 2007-06-13. http://web.archive.org/web/20070613192148/http://www.cancer.org/downloads/STT/CAFF2005BrFacspdf2005.pdf. Retrieved 2007-04-26.
- ^ a b California Environmental Protection Agency: Air Resources Board, "Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant" (June 24, 2005); on January 26, 2006, the Air Resources Board, following a lengthy review and public outreach process, determined ETS to be a Toxic Air Contaminant (TAC).
- ^ a b U.S. Department of Health and Human Services. "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General", 2006
- ^ a b J. Russo, I. Russo. "Molecular Basis of Breast Cancer: Prevention and Treatment," Springer, 2003
- ^ Cohen M, Lippman M, Chabner B (October 1978). "Role of pineal gland in aetiology and treatment of breast cancer". Lancet 2 (8094): 814–6. doi:10.1016/S0140-6736(78)92591-6. PMID 81365.
- ^ Blask DE, Brainard GC, Dauchy RT, et al. (December 2005). "Melatonin-depleted blood from premenopausal women exposed to light at night stimulates growth of human breast cancer xenografts in nude rats". Cancer Research 65 (23): 11174–84. doi:10.1158/0008-5472.CAN-05-1945. PMID 16322268.
- ^ IARC Press release No. 180
- ^ Schernhammer ES, Schulmeister K (March 2004). "Melatonin and cancer risk: does light at night compromise physiologic cancer protection by lowering serum melatonin levels?". Br. J. Cancer 90 (5): 941–3. doi:10.1038/sj.bjc.6601626. PMC 2409637. PMID 14997186. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2409637.
- ^ Hansen J (January 2001). "Increased breast cancer risk among women who work predominantly at night". Epidemiology 12 (1): 74–7. doi:10.1097/00001648-200101000-00013. PMID 11138824. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1044-3983&volume=12&issue=1&spage=74.
- ^ Hansen J (October 2001). "Light at night, shiftwork, and breast cancer risk". J. Natl. Cancer Inst. 93 (20): 1513–5. doi:10.1093/jnci/93.20.1513. PMID 11604468. http://jnci.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=11604468.
- ^ Schernhammer ES, Laden F, Speizer FE, et al. (October 2001). "Rotating night shifts and risk of breast cancer in women participating in the nurses' health study". J. Natl. Cancer Inst. 93 (20): 1563–8. doi:10.1093/jnci/93.20.1563. PMID 11604480. http://jnci.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=11604480.
- ^ Navara KJ, Nelson RJ (October 2007). "The dark side of light at night: physiological, epidemiological, and ecological consequences" (PDF). J. Pineal Res. 43 (3): 215–24. doi:10.1111/j.1600-079X.2007.00473.x. PMID 17803517. http://www.psy.ohio-state.edu/nelson/documents/JPinealRes2007.pdf.
- ^ Vainshtein, J (2008). "Disparities in breast cancer incidence across racial/ethnic strata and socioeconomic status: a systematic review". Journal of the National Medical Association 100 (7): 833–9. PMID 18672561.
- ^ Wisconsin Cancer Incidence and Mortality, 2000–2004 Wisconsin Department of Health and Family Services
- ^ a b Tammemagi CM (2007). "Racial/ethnic disparities in breast and gynecologic cancer treatment and outcomes". Curr. Opin. Obstet. Gynecol. 19 (1): 31–6. doi:10.1097/GCO.0b013e3280117cf8. PMID 17218849.
- ^ Hirschman J, Whitman S, Ansell D (2007). "The black:white disparity in breast cancer mortality: the example of Chicago". Cancer Causes Control 18 (3): 323–33. doi:10.1007/s10552-006-0102-y. PMID 17285262.
- ^ Breast cancer rates differ in races by Amanda Villa Wednesday, October 24, 2007. Badger Herald
- ^ Benjamin M, Reddy S, Brawley OW (2003). "Myeloma and race: a review of the literature". Cancer Metastasis Rev. 22 (1): 87–93. doi:10.1023/A:1022268103136. PMID 12716040.
- ^ Zuckerman, D. (2009). "The Ethics of Inclusion and Exclusion in Clinical Trials: Race, Sex, and Age". The Penn Center Guide to bioethics. (Eds:Vardit Ravitsky, Autumn Fiester, Art Caplan). Springer. ISBN 9780826115225. http://books.google.com/?id=hydXVrEWY-UC&pg=PT272&lpg=PT272&dq=The+Ethics+of+Inclusion+and+Exclusion+in+Clinical+Trials&q=The%20Ethics%20of%20Inclusion%20and%20Exclusion%20in%20Clinical%20Trials.
- ^ Demicheli R, Retsky MW, Hrushesky WJ, Baum M, Gukas ID, Jatoi I (2007). "Racial disparities in breast cancer outcome: insights into host-tumor interactions". Cancer 110 (9): 1880–8. doi:10.1002/cncr.22998. PMID 17876835.
- ^ Hausauer, A.; Keegan, T.; Chang, E.; Clarke, C. (2007). "Recent breast cancer trends among Asian/Pacific Islander, Hispanic, and African-American women in the US: changes by tumor subtype". Breast cancer research : BCR 9 (6): R90. doi:10.1186/bcr1839. PMC 2246193. PMID 18162138. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2246193.
- ^ Kumar N, Titus-Ernstoff L, Newcomb PA, Trentham-Dietz A, Anic G, Egan KM (January 2009). "Tea consumption and risk of breast cancer". Cancer Epidemiology, Biomarkers & Prevention 18 (1): 341–5. doi:10.1158/1055-9965.EPI-08-0819. PMID 19124518.
- ^ "Breast cancer: weak tea study". January 22, 2009. http://www.nhs.uk/news/2009/01January/Pages/Teaandbreastcancer.aspx. Retrieved 2009-01-22.
- ^ Ganmaa D, Willett WC, Li TY, et al. (May 2008). "Coffee, tea, caffeine and risk of breast cancer: a 22-year follow-up". International Journal of Cancer. Journal International Du Cancer 122 (9): 2071–6. doi:10.1002/ijc.23336. PMID 18183588.
- ^ Wu AH, Yu MC, Tseng CC, Hankin J, Pike MC (September 2003). "Green tea and risk of breast cancer in Asian Americans". International Journal of Cancer 106 (4): 574–9. doi:10.1002/ijc.11259. PMID 12845655.
- ^ Gierach, Gretchen L. (April 19, 2010). Relationship of mammographic density with breast cancer subtypes. http://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=6c872330-0604-4fc5-b486-6557d8ec1e5c&cKey=f0a2756e-0a22-48f3-ac30-e864d3fbedec&mKey={0591FA3B-AFEF-49D2-8E65-55F41EE8117E}. Lay summary.
- ^ Breast Density Change Linked to Cancer Development in WHI Hormone Replacement Study
- ^ Dees C, Askari M, Garrett S, Gehrs K, Henley D, Ardies CM (April 1997). "Estrogenic and DNA-damaging activity of Red No. 3 in human breast cancer cells". Environmental Health Perspectives (Environmental Health Perspectives, Vol. 105) 105 (Suppl 3): 625–32. doi:10.2307/3433381. JSTOR 3433381. PMC 1469907. PMID 9168006. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1469907.
- ^ Russo J, Russo I (1980). "Susceptibility of the mammary gland to carcinogenesis. II. Pregnancy interruption as a risk factor in tumor incidence". Am J Pathol 100 (2): 505–506. PMC 1903536. PMID 6773421. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1903536. "In contrast, abortion is associated with increased risk of carcinomas of the breast. The explanation for these epidemiologic findings is not known, but the parallelism between the DMBA-induced rat mammary carcinoma model and the human situation is striking. [...] Abortion would interrupt this process, leaving in the gland undifferentiated structures like those observed in the rat mammary gland, which could render the gland again susceptible to carcinogenesis."
- ^ "WHO | Induced abortion does not increase breast cancer risk". who.int. Archived from the original on 2007-12-14. http://web.archive.org/web/20071214064635/http://www.who.int/mediacentre/factsheets/fs240/en/index.html. Retrieved 2007-12-24.
- ^ "Politics & Science - Investigating the State of Science Under the Bush Administration". oversight.house.gov. Archived from the original on 2008-03-27. http://web.archive.org/web/20080327055020/http://oversight.house.gov/features/politics_and_science/example_breast_cancer.htm. Retrieved 2008-04-14.
- ^ "Bras and breast cancer risk". http://cancerhelp.cancerresearchuk.org/about-cancer/cancer-questions/bras-and-breast-cancer-risk.
- ^ Harding, Anne. (2006) Aluminum Salts Could Increase Breast Cancer Risk. Reuters Health.
- ^ Darbre PD (2006). "Metalloestrogens: an emerging class of inorganic xenoestrogens with potential to add to the oestrogenic burden of the human breast". Journal of Applied Toxicology 26 (3): 191–7. doi:10.1002/jat.1135. PMID 16489580.
- ^ Darbre PD (September 2005). "Aluminium, antiperspirants and breast cancer". Journal of Inorganic Biochemistry 99 (9): 1912–9. doi:10.1016/j.jinorgbio.2005.06.001. PMID 16045991.
- ^ Surendran A (2004). "Studies linking breast cancer to deodorants smell rotten, experts say". Nat. Med. 10 (3): 216. doi:10.1038/nm0304-216b. PMID 14991030.
- ^ "Antiperspirants don't cause breast cancer". Harvard Women's Health Watch 10 (5): 7. January 2003. PMID 12543590.
- ^ Potashnik G, Lerner-Geva L, Genkin L, Chetrit A, Lunenfeld E, Porath A (1999). "Fertility drugs and the risk of breast and ovarian cancers: results of a long-term follow-up study". Fertil. Steril. 71 (5): 853–9. doi:10.1016/S0015-0282(99)00085-0. PMID 10231045.
- ^ Heng, B.; Glenn, W. K.; Ye, Y.; Tran, B.; Delprado, W.; Lutze-Mann, L.; Whitaker, N. J.; Lawson, J. S. (2009). "Human papilloma virus is associated with breast cancer". British Journal of Cancer 101 (8): 1345–1350. doi:10.1038/sj.bjc.6605282. PMC 2737128. PMID 19724278. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2737128.
- ^ Harkins, L. E.; Matlaf, L. A.; Soroceanu, L.; Klemm, K.; Britt, W. J.; Wang, W.; Bland, K. I.; Cobbs, C. S. (2010). "Detection of human cytomegalovirus in normal and neoplastic breast epithelium". Herpesviridae 1 (1): 8. doi:10.1186/2042-4280-1-8. PMC 3063230. PMID 21429243. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3063230.
- ^ Lawson, J. S.; Günzburg, W. H.; Whitaker, N. J. (2006). "Viruses and human breast cancer". Future Microbiology 1 (1): 33–51. doi:10.2217/17460913.1.1.33. PMID 17661684.
- ^ Lawson, J. S.; Tran, D.; Rawlinson, W. D. (2001). "From Bittner to Barr: A viral, diet and hormone breast cancer aetiology hypothesis". Breast cancer research : BCR 3 (2): 81–85. PMC 138675. PMID 11250750. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=138675.
- ^ Taneja, P.; Frazier, D. P.; Kendig, R. D.; Maglic, D.; Sugiyama, T.; Kai, F.; Taneja, N. K.; Inoue, K. (2009). "MMTV mouse models and the diagnostic values of MMTV-like sequences in human breast cancer". Expert Review of Molecular Diagnostics 9 (5): 423–440. doi:10.1586/erm.09.31. PMC 2759974. PMID 19580428. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2759974.
- ^ a b Yalom, Marilyn (1997). A history of the breast. New York: Alfred A. Knopf. p. 234. ISBN 0-679-43459-3.
- ^ a b Olson, James Stuart (2002). Bathsheba's breast: women, cancer & history. Baltimore: The Johns Hopkins University Press. pp. 32–33. ISBN 0-8018-6936-6.
See also
- Carcinogen#IARC classification of carcinogens
- Xenoestrogen
- Your Disease Risk
External links
- Breast cancer at the Open Directory Project
- GeneReviews/NCBI/NIH/UW entry on BRCA1 and BRCA2 Hereditary Breast/Ovarian Cancer
- Breast cancer database at Silent Spring Institute
- Risk factors for breast cancer at the Open Directory Project
Tumors: breast cancer (C50/D24, 174–175/217) – Histopathologic classification Fibroepithelial/stromal Ductal, lobular, and medullary Intraductal papillomaInvasive lobular carcinoma (ILC)MedullaryOther/ungroupedPrecursor lesions Atypical ductal hyperplasiaOther Related subjects Main article · Classification · Risk factors (Alcohol · Hereditary breast-ovarian cancer syndrome · BRCA mutation) · Screening · Treatment
Pathology: Tumor, Neoplasm, Cancer, and Oncology (C00–D48, 140–239) Conditions Malignant progressionTopographyHead/Neck (Oral, Nasopharyngeal) · Digestive system · Respiratory system · Bone · Skin · Blood · Urogenital · Nervous system · Endocrine systemHistologyOtherPrecancerous condition · Paraneoplastic syndromeStaging/grading Carcinogenesis Misc. M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Categories:
Wikimedia Foundation. 2010.