- Cervix
-
Cervix 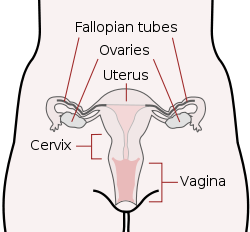
Schematic frontal view of female anatomy 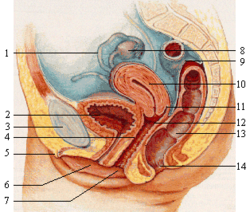
1: fallopian tube, 2: bladder, 3: pubic bone, 4: g-spot, 5: clitoris, 6: urethra, 7: vagina, 8: ovary, 9: sigmoid colon, 10: uterus, 11: fornix, 12: cervix, 13: rectum, 14: anus Latin cervix uteri Artery vaginal artery, uterine artery Precursor Müllerian duct MeSH Cervix+uteri Dorlands/Elsevier cervix uteri The cervix (from the Latin cervix uteri, meaning "neck of the womb") is the lower, narrow portion of the uterus where it joins with the top end of the vagina. It is cylindrical or conical in shape and protrudes through the upper anterior vaginal wall. Approximately half its length is visible with appropriate medical equipment; the remainder lies above the vagina beyond view.
Contents
Anatomy
Ectocervix
The portion projecting into the vagina is referred to as the portio vaginalis or ectocervix. On average, the ectocervix is 3 cm long and 2.5 cm wide. It has a convex, elliptical surface and is divided into anterior and posterior lips.
External os
Main article: External orifice of the uterusThe ectocervix's opening is called the external os. The size and shape of the external os and the ectocervix varies widely with age, hormonal state, and whether the woman has had a vaginal birth. In women who have not had a vaginal birth the external os appears as a small, circular opening. In women who have had a vaginal birth, the ectocervix appears bulkier and the external os appears wider, more slit-like and gaping.
Endocervical canal
The passageway between the external os and the uterine cavity is referred to as the endocervical canal. It varies greatly in length and width, along with the cervix overall. Flattened anterior to posterior, the endocervical canal measures 7 to 8 mm at its widest in reproductive-aged women.
Internal os
The endocervical canal terminates at the internal os which is the opening of the cervix inside the uterine cavity.
Histology
The epithelium of the cervix is varied. The ectocervix (more distal, by the vagina) is composed of nonkeratinized stratified squamous epithelium. The endocervix (more proximal, within the uterus) is composed of simple columnar epithelium.[1]
The area adjacent to the border of the endocervix and ectocervix is known as the transformation zone. The Transformation zone undergoes metaplasia numerous times during normal life. When the endocervix is exposed to the harsh acidic environment of the vagina it undergoes metaplasia to squamous epithelium which is better suited to the vaginal environment. Similarly when the ectocervix enters the less harsh uterine area it undergoes metaplasia to become columnar epithelium.
Times in life when this metaplasia of the transformation zone occurs:
- puberty; when the endocervix everts (moves out) of the uterus
- with the changes of the cervix associated with the normal menstrual cycle
- post-menopause; the uterus shrinks moving the transformation zone upwards
All these changes are normal and the occurrence is said to be physiological.
However, all this metaplasia does increase the risk of cancer in this area - the transformation zone is the most common area for cervical cancer to occur.
At certain times of life, the columnar epithelium is replaced by metaplastic squamous epithelium, and is then known as the transformation zone.
Nabothian cysts are often found in the cervix.[2]
Cervical mucus
Cervical Mucus is 90% water. Depending on the water content which varies during the menstrual cycle the mucus functions as a barrier or a transport medium to spermatoza. Cervical mucus also contains electrolytes (calcium, sodium and potassium), organic components such as glucose, amino acids and soluble proteins.[3]
Cervical mucus contains trace elements including zinc, copper, iron, mangenese and selenium, the levels of which vary dependant on cyclical hormone variation during different phases of the menstrual cycle [4] Various enzymes have been identified in human cervical mucus. Glycerol is a natural ingredient of human cervical fluid.[5][6][7][8] Studies have shown that the amount of glycerol in cervical fluid increases during sexual excitement.[6] This increase in glycerol has been postulated to be responsible for the lubricating quality of this fertile cervical fluid and may be biologically relevant during the early phase of reproductive events.
After a menstrual period ends, the external os is blocked by mucus that is thick and acidic. This "infertile" mucus blocks spermatozoa from entering the uterus.[9] For several days around the time of ovulation, "fertile" types of mucus are produced; they have a higher water content, and are less acidic and higher in electrolytes. These electrolytes cause the 'ferning' pattern that can be observed in drying mucus under low magnification; as the mucus dries, the salts crystalize, resembling the leaves of a fern.[10]
Some methods of fertility awareness involve estimating a woman's periods of fertility and infertility by observing changes in her body. Among these changes are several involving the quality of her cervical mucus: the sensation it causes at the vulva, its elasticity (Spinnbarkeit), its transparency, and the presence of ferning.[10]
Most methods of hormonal contraception work primarily by preventing ovulation, but their effectiveness is increased because they prevent the fertile types of cervical mucus from being produced. Conversely, methods of thinning the mucus may help to achieve pregnancy. One suggested method is to take guaifenesin in the few days before ovulation.[11]
During pregnancy the cervix is blocked by a special antibacterial mucosal plug which prevents infection, somewhat similar to its state during the infertile portion of the menstrual cycle. The mucus plug comes out as the cervix dilates in labor or shortly before.
Cervical position
After menstruation and directly under the influence of estrogen, the cervix undergoes a series of changes in position and texture. During most of the menstrual cycle, the cervix remains firm, like the tip of the nose, and is positioned low and closed. However, as a woman approaches ovulation, the cervix becomes softer, and rises and opens in response to the high levels of estrogen present at ovulation.[12] These changes, accompanied by the production of fertile types of cervical mucus, support the survival and movement of sperm.
Function
During menstruation the cervix stretches open slightly to allow the endometrium to be shed. This stretching is believed to be part of the cramping pain that many women experience. Evidence for this is given by the fact that some women's cramps subside or disappear after their first vaginal birth because the cervical opening has widened. During childbirth, contractions of the uterus will dilate the cervix up to 10 cm in diameter to allow the child to pass through.
During orgasm, the cervix convulses and the external os dilates. Robin Baker and Mark A. Bellis, both at the University of Manchester, first proposed that this behavior would tend to draw semen in the vagina into the uterus, increasing the likelihood of conception.[13] This explanation has been called the "upsuck theory of female orgasm." Komisaruk, Whipple, and Beyer-Flores, in their book, The Science of Orgasm, claimed there is evidence in support of the upsuck theory.[14] Science historian Elisabeth Lloyd, author of The Case of the Female Orgasm, questioned the logic of this theory and the quality of the experimental data used to back it,[15] commenting in 2005: "[The upsuck theory] has been widely accepted in the community of scientists for the past 12 years... But unfortunately the evidence for it is really badly flawed. In one of their tables 73% of the data came from one woman. It's really quite shocking that for 12 years this research has been taught as "fact" all across the US, Canada and the UK."[16]
Short cervix[17] is the strongest predictor of preterm birth.[18][19][20] Some treatments to prevent cervical cancer, such as LEEP, cold-knife conization, or cryotherapy may shorten the cervix.
Cervical cancer
Main article: Cervical cancerHuman papillomavirus (HPV) infection is a necessary factor in the development of nearly all cases of cervical cancer. HPV vaccines can reduce the chance of developing cervical cancer, if administered before initiation of sexual activity. Potentially pre-cancerous changes in the cervix can be detected by a Pap smear, in which epithelial cells are scraped from the surface of the cervix and examined under a microscope. With appropriate treatment of detected abnormalities, cervical cancer can be prevented. Most women who develop cervical cancer have never had a Pap smear, or have not had one within the last five years.
Worldwide, cervical cancer is the fifth most deadly cancer in women.[21] It affects about 16 per 100,000 women per year and kills about 9 per 100,000 per year.[22] Pap smear screening has greatly reduced cervical cancer incidence and mortality in nations with regular screening programs.
Lymphatic drainage
The lymphatic drainage of the cervix is along the uterine arteries and cardinal ligaments to the parametrial, external iliac vein, internal iliac vein, and obturator and presacral lymph nodes. From these pelvic lymph nodes, drainage then proceeds to the paraaortic lymph nodes. In some women, the lymphatics drain directly to the paraaortic nodes.
Additional images
References
- ^ Histology at BU 19404loa
- ^ Weschler, pp. 227–228.
- ^ http://www.reproduction-online.org/cgi/reprint/60/1/17.pdf, Electrolytes in vaginal fluid during the menstrual cycle of coitally active and inactive women, G. Wagner and R. J. Levin
- ^ Hagenfeldt et al., 1973;Pandey et al., 1986.
- ^ Volatile constituents of human vaginal secretions. Authors: George Huggins and George Preti (University of Pennsylvania School of Medicine). Am J Obstet Gynecol, 1976 Sep 1;126(1):129-36.
- ^ a b Alterations in the organic compounds of vaginal secretions caused by sexual arousal. Authors: George Preti, George Huggins and Geoffrey Silverberg (University of Pennsylvania School of Medicine). Fertil Steril 1979;32:47–54.
- ^ Vaginal odors and secretions. Authors: George Huggins and George Preti (University of Pennsylvania School of Medicine). Clinical Obstetrics and Gynecology, 1981; 24; 355-377.
- ^ A vaginal fluid simulant. Authors: Derek Owen and David Katz (Duke University). Contraception, 1999 Feb;59(2):91-5.
- ^ Ann Westinore; Evelyn, Dr Billings (1998). The Billings Method: Controlling Fertility Without Drugs or Devices. Toronto: Life Cycle Books. pp. 37. ISBN 0-919225-17-9.
- ^ a b Weschler, pp. 58–59.
- ^ Weschler, p. 173.
- ^ Weschler, Toni, MPH, Taking Charge of Your Fertility, Second Edition, 2002, pp. 59, 64.
- ^ Singh D, Meyer W, Zambarano RJ, Hurlbert DF (February 1998). "Frequency and timing of coital orgasm in women desirous of becoming pregnant". Arch Sex Behav 27 (1): 15–29. doi:10.1023/A:1018653724159. PMID 9494687.
- ^ Whipple, Beverly; Komisaruk, Barry R.; Beyer, Carlos; Carlos Beyer-Flores (2006). The science of orgasm. Baltimore: Johns Hopkins University Press. ISBN 0-8018-8490-X.
- ^ Lloyd, Elisabeth Anne (2006). The Case of the Female Orgasm: Bias in the Science of Evolution. Cambridge: Harvard University Press. ISBN 0-674-02246-7.
- ^ "The ideas interview: Elisabeth Lloyd". The Guardian (London). 2005-09-26. http://www.guardian.co.uk/science/2005/sep/26/genderissues.technology. Retrieved 2010-04-28.
- ^ Goldenberg RL, Iams JD, Mercer BM, et al. (1998). "The preterm prediction study: the value of new vs standard risk factors in predicting early and all spontaneous preterm births. NICHD MFMU Network". Am J Public Health 88 (2): 233–8. doi:10.2105/AJPH.88.2.233. PMC 1508185. PMID 9491013. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1508185.
- ^ To MS, Skentou CA, Royston P, Yu CKH, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: a population-based prospective study. Ultra Obstet Gynecol 2006; 27: 362–367.
- ^ Fonseca et al. Progesterone and the risk of preterm birth among women with a short cervix. NEJM 2007; vol 357, no 5, pg 462–469.
- ^ Romero R. Prevention of sponatneous preterm birth: the role of sonographic cervical length in identifying patients who may benefit from progesterone treatment. Ultrasound Obstet Gynecol 2007; 30: 675–686. http://www3.interscience.wiley.com/journal/99020267/home free download
- ^ World Health Organization (February 2006). "Fact sheet No. 297: Cancer". http://www.who.int/mediacentre/factsheets/fs297/en/index.html. Retrieved 2007-12-01.
- ^ "GLOBOCAN 2002 database: summary table by cancer". Archived from the original on 2008-06-16. http://web.archive.org/web/20080616085344/http://www-dep.iarc.fr/GLOBOCAN/Table1_sel1.htm. Retrieved 2008-10-26.
External links
- My Beautiful Cervix—site with a series of photographs illustrating the cervix over a menstrual cycle
Female reproductive system (TA A09.1–2, TH H3.07.01, GA 11.1254) Internal Adnexacorpus (hemorrhagicum, luteum, albicans) · Theca of follicle (externa, interna) · Follicular antrum (Follicular fluid) · Corona radiata · Zona pellucida · Membrana granulosa · Perivitelline spaceOtherProper of ovary · Suspensory of ovarycorpus/body (Uterine cavity, Fundus) · cervix/neck (External orifice, Canal of the cervix, Internal orifice, Supravaginal portion of cervix, Vaginal portion of cervix, Cervical ectropion) · Uterine hornsGeneralExternal Mons pubis · Labia majora (Anterior commissure, Posterior commissure) · Pudendal cleft · Labia minora (Frenulum of labia minora, Frenulum of clitoris) · Vulval vestibule · Interlabial sulci · Bulb of vestibule · Vaginal orifice
vestibular glands/ducts (Bartholin's glands/Bartholin's ducts, Skene's glands/Skene's ducts)Other Menstrual cycle Events and phases Life stages Tracking SignsSystemsSuppression Disorders Related events In culture and religion Categories:- Female reproductive system
- Latin words and phrases
Wikimedia Foundation. 2010.








