- Cancer
-
For other uses, see Cancer (disambiguation).
Cancer Classification and external resources 
A coronal CT scan showing a cancer of right pleural membranes, the outer surface of the lung and inner surface of the chest wall, malignant mesothelioma
Legend: → tumor ←, ★ central pleural effusion, 1 & 3 lungs, 2 spine, 4 ribs, 5 aorta, 6 spleen, 7 & 8 kidneys, 9 liver.ICD-10 D00 ICD-9 140—239 DiseasesDB 28843 MedlinePlus 001289 MeSH D009369 Cancer /ˈkænsər/ (
 listen), known medically as a malignant neoplasm, is a term for a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the body through the lymphatic system or bloodstream. Not all tumors are cancerous. Benign tumors do not grow uncontrollably, do not invade neighbouring tissues, and do not spread throughout the body.
listen), known medically as a malignant neoplasm, is a term for a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the body through the lymphatic system or bloodstream. Not all tumors are cancerous. Benign tumors do not grow uncontrollably, do not invade neighbouring tissues, and do not spread throughout the body.Healthy cells control their own growth and will destroy themselves if they become unhealthy. Cell division is a complex process that is normally tightly regulated. Cancer occurs when problems in the genes of a cell prevent these controls from functioning properly. These problems may come from damage to the gene or may be inherited, and can be caused by various sources inside or outside of the cell. Faults in two types of genes are especially important: oncogenes, which drive the growth of cancer cells, and tumor suppressor genes, which prevent cancer from developing.
Determining what causes cancer is complex, and it is often impossible to assign a specific cause for a specific cancer. Many things are known to increase the risk of cancer, including tobacco use, infection, radiation, lack of physical activity, poor diet and obesity, and environmental pollutants.[1] These can directly damage genes or combine with existing genetic faults within cells to cause the disease.[2] A small percentage of cancers, approximately five to ten percent, are entirely hereditary.
Cancer can be detected in a number of ways, including the presence of certain signs and symptoms, screening tests, or medical imaging. Once a possible cancer is detected it is diagnosed by microscopic examination of a tissue sample. Cancer is usually treated with chemotherapy, radiation therapy and surgery. The chances of surviving the disease vary greatly by the type and location of the cancer and the extent of disease at the start of treatment. While cancer can affect people of all ages, and a few types of cancer are more common in children, the risk of developing cancer generally increases with age. In 2007, cancer caused about 13% of all human deaths worldwide (7.9 million). Rates are rising as more people live to an old age and as mass lifestyle changes occur in the developing world.[3]
Contents
Classification
Further information: List of cancer types and List of oncology-related termsCancers are classified by the type of cell that the tumor resembles and is therefore presumed to be the origin of the tumor. These types include:
- Carcinoma: Cancers derived from epithelial cells. This group includes many of the most common cancers, particularly in the aged, and include nearly all those developing in the breast, prostate, lung, pancreas, and colon.
- Sarcoma: Cancers arising from connective tissue (i.e. bone, cartilage, fat, nerve), each of which develop from cells originating in mesenchymal cells outside the bone marrow.
- Lymphoma and leukemia: These two classes of cancer arise from hematopoietic (blood-forming) cells that leave the marrow and tend to mature in the lymph nodes and blood, respectively.
- Germ cell tumor: Cancers derived from pluripotent cells, most often presenting in the testicle or the ovary (seminoma and dysgerminoma, respectively).
- Blastoma: Cancers derived from immature "precursor" cells or embryonic tissue. These are also most common in children.[citation needed]
Cancers are usually named using -carcinoma, -sarcoma or -blastoma as a suffix, with the Latin or Greek word for the organ or tissue of origin as the root. For example, cancers of the liver parenchyma arising from malignant epithelial cells is called hepatocarcinoma, while a malignancy arising from primitive liver precursor cells is called a hepatoblastoma, and a cancer arising from fat cells is called a liposarcoma. For some common cancers, the English organ name is used. For example, the most common type of breast cancer is called ductal carcinoma of the breast. Here, the adjective ductal refers to the appearance of the cancer under the microscope, which suggests that it has originated in the milk ducts.
Benign tumors (which are not cancers) are named using -oma as a suffix with the organ name as the root. For example, a benign tumor of smooth muscle cells is called a leiomyoma (the common name of this frequently occurring benign tumor in the uterus is fibroid). Confusingly, some types of cancer also use the -oma suffix, examples including melanoma and seminoma.
Some types of cancer are named for the size and shape of the cells under a microscope, such as giant cell carcinoma, spindle cell carcinoma, and small cell carcinoma.
Signs and symptoms
Cancer symptoms can be divided into three groups:
- Local symptoms: are restricted to the site of the primary cancer. They can include lumps or swelling (tumor), hemorrhage (bleeding from the skin, mouth or anus), ulceration and pain. Although local pain commonly occurs in advanced cancer, the initial swelling is often painless.
- Metastatic symptoms: are due to the spread of cancer to other locations in the body. They can include enlarged lymph nodes (which can be felt or sometimes seen under the skin), hepatomegaly (enlarged liver) or splenomegaly (enlarged spleen) which can be felt in the abdomen, pain or fracture of affected bones, and neurological symptoms.
- Systemic symptoms: occur due to distant effects of the cancer that are not related to direct or metastatic spread. Some of these effects can include weight loss (poor appetite and cachexia), fatigue, excessive sweating (especially night sweats), anemia (low red blood cell count) and other specific conditions termed paraneoplastic phenomena. These may be mediated by immunological or hormonal signals from the cancer cells.
None of these non-specific symptoms are helpful in determining if a patient has cancer, as many of these symptoms commonly occur in individuals who do not have cancer.
Causes
It is almost always impossible to prove exactly what caused a cancer in any individual, because most cancers have multiple possible causes. For example, if a person who uses tobacco heavily develops lung cancer, then it was very probably caused by the tobacco use, but since everyone has a small chance of developing lung cancer as a result of air pollution or radiation, then there is a tiny chance that the smoker's lung cancer actually developed because of air pollution or radiation.
Cancers are primarily an environmental disease with 90-95% of cases attributed to environmental factors and 5-10% due to genetics.[1] Environmental, as used by cancer researchers, means any cause that is not genetic, not merely pollution. Common environmental factors that contribute to cancer death include tobacco (25-30%), diet and obesity (30-35%), infections (15-20%), radiation (both ionizing and non-ionizing, up to 10%), stress, lack of physical activity, and environmental pollutants.[1]
Chemicals
Further information: Alcohol and cancer and Smoking and cancerCancer pathogenesis is traceable back to DNA mutations that impact cell growth and metastasis. Substances that cause DNA mutations are known as mutagens, and mutagens that cause cancers are known as carcinogens. Particular substances have been linked to specific types of cancer. Tobacco smoking is associated with many forms of cancer,[5] and causes 90% of lung cancer.[6]
Many mutagens are also carcinogens, but some carcinogens are not mutagens. Alcohol is an example of a chemical carcinogen that is not a mutagen.[7] In Western Europe 10% of cancers in males and 3% of cancers in females are attributed to alcohol.[8]
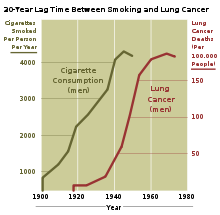
Decades of research has demonstrated the link between tobacco use and cancer in the lung, larynx, head, neck, stomach, bladder, kidney, esophagus and pancreas.[9] Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.[10] Tobacco is responsible for about one in three of all cancer deaths in the developed world,[5] and about one in five worldwide.[10] Lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently,[when?] decreases in smoking followed by decreases in lung cancer death rates in men. However, the numbers of smokers worldwide is still rising, leading to what some organizations have described as the tobacco epidemic.[11]
Cancer related to one's occupation is believed to represent between 2–20% of all cases.[12] Every year, at least 200,000 people die worldwide from cancer related to their workplace.[13] Currently,[when?] most cancer deaths caused by occupational risk factors occur in the developed world.[13] It is estimated that approximately 20,000 cancer deaths and 40,000 new cases of cancer each year in the U.S. are attributable to occupation.[14] Millions of workers run the risk of developing cancers such as lung cancer and mesothelioma from inhaling asbestos fibers and tobacco smoke, or leukemia from exposure to benzene at their workplaces.[13]
Diet and exercise
Diet, physical inactivity, and obesity are related to approximately 30–35% of cancer cases.[1][15] In the United States excess body weight is associated with the development of many types of cancer and is a factor in 14–20% of all cancer deaths.[15] Physical inactivity is believed to contribute to cancer risk not only through its effect on body weight but also through negative effects on immune system and endocrine system.[15]
Diets that are low in vegetables, fruits and whole grains, and high in processed or red meats are linked with a number of cancers.[15] A high salt diet is linked to gastric cancer, aflatoxin B1, a frequent food contaminate, with liver cancer, and Betel nut chewing with oral cancer.[16] This may partly explain differences in cancer incidence in different countries for example gastric cancer is more common in Japan with its high salt diet[17] and colon cancer is more common in the United States. Immigrants develop the risk of their new country, often within one generation, suggesting a substantial link between diet and cancer.[18]
Infection
Main article: Infectious causes of cancerWorldwide approximately 18% of cancers are related to infectious diseases.[1] This proportion varies in different regions of the world from a high of 25% in Africa to less than 10% in the developed world.[1] Viruses are usual infectious agents that cause cancer but bacteria and parasites may also have an effect.
A virus that can cause cancer is called an oncovirus. These include human papillomavirus (cervical carcinoma), Epstein-Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma), Kaposi's sarcoma herpesvirus (Kaposi's Sarcoma and primary effusion lymphomas), hepatitis B and hepatitis C viruses (hepatocellular carcinoma), and Human T-cell leukemia virus-1 (T-cell leukemias). Bacterial infection may also increase the risk of cancer, as seen in Helicobacter pylori-induced gastric carcinoma.[19] Parasitic infections strongly associated with cancer include Schistosoma haematobium (squamous cell carcinoma of the bladder) and the liver flukes, Opisthorchis viverrini and Clonorchis sinensis (cholangiocarcinoma).[20]
Radiation
Up to 10% of invasive cancers are related to radiation exposure, including both ionizing radiation and non-ionizing radiation.[1] Additionally, the vast majority of non-invasive cancers are non-melanoma skin cancers caused by non-ionizing radiation from ultraviolet radiation.
Sources of ionizing radiation include medical imaging, and radon gas. Radiation can cause cancer in most parts of the body, in all animals, and at any age, although radiation-induced solid tumors usually take 10–15 years, and can take up to 40 years, to become clinically manifest, and radiation-induced leukemias typically require 2–10 years to appear.[21] Some people, such as those with nevoid basal cell carcinoma syndrome or retinoblastoma, are more susceptible than average to developing cancer from radiation exposure.[21] Children and adolescents are twice as likely to develop radiation-induced leukemia as adults; radiation exposure before birth has ten times the effect.[21] Ionizing radiation is not a particularly strong mutagen.[21] Residential exposure to radon gas, for example, has similar cancer risks as passive smoking.[21] Low-dose exposures, such as living near a nuclear power plant, are generally believed to have no or very little effect on cancer development.[21] Radiation is a more potent source of cancer when it is combined with other cancer-causing agents, such as radon gas exposure plus smoking tobacco.[21]
Unlike chemical or physical triggers for cancer, ionizing radiation hits molecules within cells randomly. If it happens to strike a chromosome, it can break the chromosome, result in an abnormal number of chromosomes, inactivate one or more genes in the part of the chromosome that it hit, delete parts of the DNA sequence, cause chromosome translocations, or cause other types of chromosome abnormalities.[21] Major damage normally results in the cell dying, but smaller damage may leave a stable, partly functional cell that may be capable of proliferating and developing into cancer, especially if tumor suppressor genes were damaged by the radiation.[21] Three independent stages appear to be involved in the creation of cancer with ionizing radiation: morphological changes to the cell, acquiring cellular immortality (losing normal, life-limiting cell regulatory processes), and adaptations that favor formation of a tumor.[21] Even if the radiation particle does not strike the DNA directly, it triggers responses from cells that indirectly increase the likelihood of mutations.[21]
Medical use of ionizing radiation is a growing source of radiation-induced cancers. Ionizing radiation may be used to treat other cancers, but this may, in some cases, induce a second form of cancer.[21] It is also used in some kinds of medical imaging. One report estimates that approximately 29,000 future cancers could be related to the approximately 70 million CT scans performed in the US in 2007.[22] It is estimated that 0.4% of current[when?] cancers in the United States are due to CTs performed in the past and that this may increase to as high as 1.5–2% with 2007 rates of CT usage.[23]
Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies.[24] Clear evidence establishes ultraviolet radiation, especially the non-ionizing medium wave UVB, as the cause of most non-melanoma skin cancers, which are the most common forms of cancer in the world.[24]
Non-ionizing radio frequency radiation from mobile phones, electric power transmission, and other similar sources have been described as a possible carcinogen by the World Health Organization's International Agency for Research on Cancer.[25]
Heredity
Main article: Cancer syndromeThe vast majority of cancers are non-hereditary, which are called sporadic cancers. Hereditary cancers are cancers that are primarily caused by an inherited genetic defect. Less than 0.3% of the population are carriers of a genetic mutation which has a large effect on cancer risk.[26] They cause less than 3–10% of all cancer.[26] Some of these syndromes include:
- certain inherited mutations in the genes BRCA1 and BRCA2 with a more than 75% risk of breast cancer and ovarian cancer[26]
- Li-Fraumeni syndrome (various tumors such as osteosarcoma, breast cancer, soft tissue sarcoma, brain tumors) due to mutations of p53
- Turcot syndrome (brain tumors and colonic polyposis)
- Familial adenomatous polyposis an inherited mutation of the APC gene that leads to early onset of colon carcinoma.
- Hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch syndrome) can include familial cases of colon cancer, uterine cancer, gastric cancer, and ovarian cancer, without a preponderance of colon polyps.
- Retinoblastoma, when occurring in young children, is due to a hereditary mutation in the retinoblastoma gene.
- Down syndrome patients, who have an extra chromosome 21, are known to develop malignancies such as leukemia and testicular cancer, though the reasons for this difference are not well understood.
Physical agents
Some substances cause cancer primarily through their physical, rather than chemical, effects on cells.[27]
A prominent example of this is prolonged exposure to asbestos, naturally occurring mineral fibers which are a major cause of mesothelioma, a type of lung cancer.[27] Other substances in this category include both naturally occurring and synthetic asbestos-like fibers, such as wollastonite, attapulgite, glass wool, and rock wool, are believed to have similar effects.[27]
Nonfibrous particulate materials that cause cancer include powdered metallic cobalt and nickel, and crystalline silica (quartz, cristobalite, and tridymite).[27]
Usually, physical carcinogens must get inside the body (such as through inhaling tiny pieces) and require years of exposure to develop cancer.[27]
Physical trauma and inflammation
Physical trauma resulting in cancer is relatively rare.[28] Claims that breaking bone resulted in bone cancer, for example, have never been proven.[28] Similarly, physical trauma is not accepted as a cause for cervical cancer, breast cancer, or brain cancer.[28]
One accepted source is frequent, long-term application of hot objects to the body. It is possible that repeated burns on the same part of the body, such as those produced by kanger and kairo heaters (charcoal hand warmers), may produce skin cancer, especially if carcinogenic chemicals are also present.[28] Frequently drinking scalding hot tea may produce esophageal cancer.[28]
Generally, it is believed that the cancer arises, or a pre-existing cancer is encouraged, during the process of repairing the trauma, rather than the cancer being caused directly by the trauma.[28] However, repeated injuries to the same tissues might promote excessive cell proliferation, which could then increase the odds of a cancerous mutation. There is no evidence that inflammation itself causes cancer.[28]
Hormones
Some hormones factor in the development of cancer by promoting cell proliferation.[29] Hormones are important agents in sex-related cancers such as cancer of the breast, endometrium, prostate, ovary, and testis, and also of thyroid cancer and bone cancer.[29]
An individual's hormone levels are mostly determined genetically, so this may at least partly explains the presence of some cancers that run in families that do not seem to have any cancer-causing genes.[29] For example, the daughters of women who have breast cancer have significantly higher levels of estrogen and progesterone than the daughters of women without breast cancer. These higher hormone levels may explain why these women have higher risk of breast cancer, even in the absence of a breast-cancer gene.[29] Similarly, men of African ancestry have significantly higher levels of testosterone than men of European ancestry, and have a correspondingly much higher level of prostate cancer.[29] Men of Asian ancestry, with the lowest levels of testosterone-activating androstanediol glucuronide, have the lowest levels of prostate cancer.[29]
However, non-genetic factors are also relevant: obese people have higher levels of some hormones associated with cancer and a higher rate of those cancers.[29] Women who take hormone replacement therapy have a higher risk of developing cancers associated with those hormones.[29] On the other hand, people who exercise far more than average have lower levels of these hormones, and lower risk of cancer.[29] Osteosarcoma may be promoted by growth hormones.[29] Some treatments and prevention approaches leverage this cause by artificially reducing hormone levels, and thus discouraging hormone-sensitive cancers.[29]
Other
Excepting the rare transmissions that occur with pregnancies and only a marginal few organ donors, cancer is generally not a transmissible disease. The main reason for this is tissue graft rejection caused by MHC incompatibility.[30] In humans and other vertebrates, the immune system uses MHC antigens to differentiate between "self" and "non-self" cells because these antigens are different from person to person. When non-self antigens are encountered, the immune system reacts against the appropriate cell. Such reactions may protect against tumour cell engraftment by eliminating implanted cells. In the United States, approximately 3,500 pregnant women have a malignancy annually, and transplacental transmission of acute leukaemia, lymphoma, melanoma and carcinoma from mother to fetus has been observed.[30] The development of donor-derived tumors from organ transplants is exceedingly rare. The main cause of organ transplant associated tumors seems to be malignant melanoma, that was undetected at the time of organ harvest.[31] though other cases exist[32] In fact, cancer from one organism will usually grow in another organism of that species, as long as they share the same histocompatibility genes,[33] proven using mice; however this would never happen in a real-world setting except as described above.
In non-humans, a few types of transmissible cancer have been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with Sticker's sarcoma, also known as canine transmissible venereal tumor,[34] as well as devil facial tumour disease in Tasmanian devils.
Pathophysiology
Main articles: Carcinogenesis and The Hallmarks of Cancer Cancers are caused by a series of mutations. Each mutation alters the behavior of the cell somewhat.
Cancers are caused by a series of mutations. Each mutation alters the behavior of the cell somewhat.
Cancer is fundamentally a disease of failure of regulation of tissue growth. In order for a normal cell to transform into a cancer cell, the genes which regulate cell growth and differentiation must be altered.[35]
The affected genes are divided into two broad categories. Oncogenes are genes which promote cell growth and reproduction. Tumor suppressor genes are genes which inhibit cell division and survival. Malignant transformation can occur through the formation of novel oncogenes, the inappropriate over-expression of normal oncogenes, or by the under-expression or disabling of tumor suppressor genes. Typically, changes in many genes are required to transform a normal cell into a cancer cell.[36]
Genetic changes can occur at different levels and by different mechanisms. The gain or loss of an entire chromosome can occur through errors in mitosis. More common are mutations, which are changes in the nucleotide sequence of genomic DNA.
Large-scale mutations involve the deletion or gain of a portion of a chromosome. Genomic amplification occurs when a cell gains many copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material. Translocation occurs when two separate chromosomal regions become abnormally fused, often at a characteristic location. A well-known example of this is the Philadelphia chromosome, or translocation of chromosomes 9 and 22, which occurs in chronic myelogenous leukemia, and results in production of the BCR-abl fusion protein, an oncogenic tyrosine kinase.
Small-scale mutations include point mutations, deletions, and insertions, which may occur in the promoter region of a gene and affect its expression, or may occur in the gene's coding sequence and alter the function or stability of its protein product. Disruption of a single gene may also result from integration of genomic material from a DNA virus or retrovirus, and resulting in the expression of viral oncogenes in the affected cell and its descendants.
Replication of the enormous amount of data contained within the DNA of living cells will probabilistically result in some errors (mutations). Complex error correction and prevention is built into the process, and safeguards the cell against cancer. If significant error occurs, the damaged cell can "self-destruct" through programmed cell death, termed apoptosis. If the error control processes fail, then the mutations will survive and be passed along to daughter cells.
Some environments make errors more likely to arise and propagate. Such environments can include the presence of disruptive substances called carcinogens, repeated physical injury, heat, ionising radiation, or hypoxia[37] (see causes, below).
The errors which cause cancer are self-amplifying and compounding, for example:
- A mutation in the error-correcting machinery of a cell might cause that cell and its children to accumulate errors more rapidly.
- A further mutation in an oncogene might cause the cell to reproduce more rapidly and more frequently than its normal counterparts.
- A further mutation may cause loss of a tumour suppressor gene, disrupting the apoptosis signalling pathway and resulting in the cell becoming immortal.
- A further mutation in signaling machinery of the cell might send error-causing signals to nearby cells.
The transformation of normal cell into cancer is akin to a chain reaction caused by initial errors, which compound into more severe errors, each progressively allowing the cell to escape the controls that limit normal tissue growth. This rebellion-like scenario becomes an undesirable survival of the fittest, where the driving forces of evolution work against the body's design and enforcement of order. Once cancer has begun to develop, this ongoing process, termed clonal evolution drives progression towards more invasive stages.[38]
Diagnosis
Most cancers are initially recognized either because signs or symptoms appear or through cancer screening. Neither of these lead to a definitive diagnosis, which usually requires the opinion of a pathologist, a type of physician (medical doctor) who specializes in the diagnosis of cancer and other diseases. People with suspected cancer are investigated with medical tests. These commonly include blood tests, X-rays, CT scans and endoscopy.
Pathology
A cancer may be suspected for a variety of reasons, but the definitive diagnosis of most malignancies must be confirmed by histological examination of the cancerous cells by a pathologist. Tissue can be obtained from a biopsy or surgery. Many biopsies (such as those of the skin, breast or liver) can be done in a doctor's office. Biopsies of other organs are performed under anesthesia and require surgery in an operating room.
The tissue diagnosis given by the pathologist indicates the type of cell that is proliferating, its histological grade, genetic abnormalities, and other features of the tumor. Together, this information is useful to evaluate the prognosis of the patient and to choose the best treatment. Cytogenetics and immunohistochemistry are other types of testing that the pathologist may perform on the tissue specimen. These tests may provide information about the molecular changes (such as mutations, fusion genes, and numerical chromosome changes) that has happened in the cancer cells, and may thus also indicate the future behavior of the cancer (prognosis) and best treatment.
-
An invasive ductal carcinoma of the breast (pale area at the center) surrounded by spikes of whitish scar tissue in the surrounding yellow fatty tissue.
-
An invasive colorectal carcinoma (top center) in a colectomy specimen.
-
A squamous cell carcinoma (the whitish tumor) near the bronchi in a lung specimen.
-
A large invasive ductal carcinoma in a mastectomy specimen.
Prevention
Cancer prevention is defined as active measures to decrease the risk of cancer.[39] The vast majority of cancer risk factors are due to environmental (including lifestyle) factors, and many of these factors are controllable. Thus, cancer is largely considered a preventable disease.[40] Greater than 30% of cancer is considered preventable by avoiding risk factors including: tobacco, overweight / obesity, an insufficient diet, physical inactivity, alcohol, sexually transmitted infections, and air pollution.[41] Not all environmental causes can be prevented. For example, exposure to naturally occurring background radiation cannot be prevented.
Dietary
Main article: Diet and cancerDietary recommendations to reduce the risk of developing cancer, including: (1) reducing intake of foods and drinks that promote weight gain, namely energy-dense foods and sugary drinks, (2) eating mostly foods of plant origin, (3) limiting intake of red meat and avoiding processed meat, (4) limiting consumption of alcoholic beverages, and (5) reducing intake of salt and avoiding mouldy cereals (grains) or pulses (legumes).[42][43]
Proposed dietary interventions for cancer risk reduction generally gain support from epidemiological association studies. Examples of such studies include reports that reduced meat consumption is associated with decreased risk of colon cancer,[44] and reports that consumption of coffee is associated with a reduced risk of liver cancer.[45] Studies have linked consumption of grilled meat to an increased risk of stomach cancer,[46] colon cancer,[47] breast cancer,[48] and pancreatic cancer,[49] a phenomenon which could be due to the presence of carcinogens in foods cooked at high temperatures.[50] Whether reducing obesity in a population also reduces cancer incidence is unknown. Some studies have found that consuming lots of fruits and vegetables has little if any effect on preventing cancer.[51] A 2005 secondary prevention study showed that consumption of a plant-based diet and lifestyle changes resulted in a reduction in cancer markers in a group of men with prostate cancer who were using no conventional treatments at the time.[52] These results were amplified by a 2006 study. Over 2,400 women were studied, half randomly assigned to a normal diet, the other half assigned to a diet containing less than 20% calories from fat. The women on the low fat diet were found to have a markedly lower risk of breast cancer recurrence, in the interim report of December, 2006.[53]
Medication
The concept that medications could be used to prevent cancer is an attractive one, and many high-quality clinical trials support the use of such chemoprevention in defined circumstances. Aspirin has been found to reduce the risk of death from cancer.[54] Daily use of tamoxifen or raloxifene has been demonstrated to reduce the risk of developing breast cancer in high-risk women by about 50%.[55]Finasteride has been shown to lower the risk of prostate cancer, though it seems to mostly prevent low-grade tumors.[56] The effect of COX-2 inhibitors such as rofecoxib and celecoxib upon the risk of colon polyps have been studied in familial adenomatous polyposis patients[57] and in the general population.[58][59] In both groups, there were significant reductions in colon polyp incidence, but this came at the price of increased cardiovascular toxicity.
Vitamins have not been found to be effective at preventing cancer,[60] although low levels of vitamin D are correlated with increased cancer risk.[61][62] Whether this relationship is causal and vitamin D supplementation is protective is yet to be determined.[63] Beta-carotene supplementation has been found to increase slightly, but not significantly, risks of lung cancer.[64] Folic acid supplementation has not been found effective in preventing colon cancer and may increase colon polyps.[65]
Vaccination
Vaccines have been developed that prevent some infection by some viruses that are associated with cancer, and therapeutic vaccines are in development[when?] to stimulate an immune response against cancer-specific epitopes.[66] Human papillomavirus vaccine (Gardasil and Cervarix) decreases the risk of developing cervical cancer.[66] The hepatitis B vaccine prevents infection with hepatitis B virus and thus decreases the risk of liver cancer.[66]
Advances in cancer research have made a vaccine designed to prevent cancers available. In 2006, the U.S. Food and Drug Administration (FDA) approved a human papilloma virus vaccine, called Gardasil. The vaccine protects against 6,11,16,18 strains of HPV, which together cause 70% of cervical cancers and 90% of genital warts. It also lists vaginal and vulvar cancers as being protected. In March 2007, the US Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) officially recommended that females aged 11–12 receive the vaccine, and indicated that females as young as age 9 and as old as age 26 are also candidates for immunization. There is a second vaccine from Cervarix which protects against the more dangerous HPV 16,18 strains only. In 2009, Gardasil was approved for protection against genital warts. In 2010, the Gardasil vaccine was approved for protection against anal cancer for males and reviewers stated there was no anatomical, histological or physiological anal differences between the genders so females would also be protected.
Screening
Main article: Cancer screeningUnlike diagnosis efforts prompted by symptoms and medical signs, cancer screening involves efforts to detect cancer after it has formed, but before any noticeable symptoms appear.[67] This may involve physical examination, blood or urine tests, or medical imaging.[67]
Cancer screening is not currently[when?] possible for some types of cancers, and even when tests are available, they are not recommended to everyone. Universal screening or mass screening involves screening everyone.[68] Selective screening identifies people who are known to be at higher risk of developing cancer, such as people with a family history of cancer.[68]
Several factors are considered to determine whether the benefits of screening outweigh the risks and the costs of screening.[67] These factors include:
- Possible harms from the screening test: Some types of screening tests, such as X-ray images, expose the body to potentially harmful ionizing radiation. There is a small chance that the radiation in the test could cause a new cancer in a healthy person. Screening mammography, used to detect breast cancer, is not recommended to men or to young women because they are more likely to be harmed by the test than to benefit from it. Other tests, such as a skin check for skin cancer, have no significant risk of harm to the patient. A test that has high potential harms is only recommended when the benefits are also high.
- The likelihood of the test correctly identifying cancer: If the test is not sensitive, then it may miss cancers. If the test is not specific, then it may wrongly indicate cancer in a healthy person. All cancer screening tests produce both false positives and false negatives, and most produce more false positives. Experts consider the rate of errors when making recommendations about which test, if any, to use. A test may work better in some populations than others. The positive predictive value is a calculation of the likelihood that a positive test result actually represents cancer in a given individual, based on the results of people with similar risk factors.
- The likelihood of cancer being present: Screening is not normally useful for rare cancers. It is rarely done for young people, since cancer is largely a disease found in people over the age of 50. Countries often focus their screening recommendations on the major forms of treatable cancer found in their population. For example, the United States recommends universal screening for colon cancer, which is common in the US, but not for stomach cancer, which is less common; by contrast, Japan recommends screening for stomach cancer, but not colon cancer, which is rarer in Japan. Screening recommendations depend on the individual's risk, with high-risk people receiving earlier and more frequent screening than low-risk people.
- Possible harms from follow-up procedures: If the screening test is positive, further diagnostic testing is normally done, such as a biopsy of the tissue. If the test produces many false positives, then many people will undergo needless medical procedures, some of which may be dangerous.
- Whether suitable treatment is available and appropriate: Screening is discouraged if no effective treatment is available.[68] When effective and suitable treatment is not available, then diagnosis of a fatal disease produces significant mental and emotional harms. For example, routine screening for cancer is typically not appropriate in a very frail elderly person, because the treatment for any cancer that is detected might kill the patient.
- Whether early detection improves treatment outcomes: Even when treatment is available, sometimes early detection does not improve the outcome. If the treatment result is the same as if the screening had not been done, then the only screening program does is increase the length of time the person lived with the knowledge that he had cancer. This phenomenon is called lead-time bias. A useful screening program reduces the number of years of potential life lost (longer lives) and disability-adjusted life years lost (longer healthy lives).
- Whether the cancer will ever need treatment: Diagnosis of a cancer in a person who will never be harmed by the cancer is called overdiagnosis. Overdiagnosis is most common among older people with slow-growing cancers. Concerns about overdiagnosis are common for breast and prostate cancer.
- Whether the test is acceptable to the patients:If a screening test is too burdensome, such as requiring too much time, too much pain, or culturally unacceptable behaviors, then people will refuse to participate.[68]
- Cost of the test: Some expert bodies, such as the U.S. Preventive Services Task Force, completely ignore the question of money. Most, however, include a cost-effectiveness analysis that, all else being equal, favors less expensive tests over more expensive tests, and attempt to balance the cost of the screening program against the benefits of using those funds for other health programs. These analyses usually include the total cost of the screening program to the healthcare system, such as ordering the test, performing the test, reporting the results, and biopsies for suspicious results, but not usually the costs to the individual, such as for time taken away from employment.
Recommendations
The U.S. Preventive Services Task Force (USPSTF) strongly recommends cervical cancer screening in women who are sexually active and have a cervix at least until the age of 65.[69] They recommend that Americans be screened for colorectal cancer via fecal occult blood testing, sigmoidoscopy, or colonoscopy starting at age 50 until age 75.[70] There is insufficient evidence to recommend for or against screening for skin cancer,[71] oral cancer,[72] lung cancer,[73] or prostate cancer in men under 75.[74] Routine screening is not recommended for bladder cancer,[75] testicular cancer,[76] ovarian cancer,[77] pancreatic cancer,[78] or prostate cancer.[79]
The USPSTF recommends mammography for breast cancer screening every two years for those 50–74 years old; however, they do not recommend either breast self-examination or clinical breast examination.[80] A 2009 Cochrane review came to slightly different conclusions with respect to breast cancer screening stating that routine mammography may do more harm than good.[81]
Japan screens for gastric cancer using photofluorography due to the high incidence there.[3]
Genetic testing
See also: Cancer syndromeGene Cancer types BRCA1, BRCA2 Breast, ovarian, pancreatic HNPCC, MLH1, MSH2, MSH6, PMS1, PMS2 Colon, uterine, small bowel, stomach, urinary tract Genetic testing for individuals at high-risk of certain cancers is recommended.[82] Carriers of these mutations may than undergo enhanced surveillance, chemoprevention, or preventative surgery to reduce their subsequent risk.[82]
Management
Main article: Management of cancerMany management options for cancer exist including: chemotherapy, radiation therapy, surgery, immunotherapy, monoclonal antibody therapy and other methods. Which treatments are used depends upon the type of cancer, the location and grade of the tumor, and the stage of the disease, as well as the general state of a person's health.
Complete removal of the cancer without damage to the rest of the body is the goal of treatment for most cancers. Sometimes this can be accomplished by surgery, but the propensity of cancers to invade adjacent tissue or to spread to distant sites by microscopic metastasis often limits its effectiveness. Surgery often required the removal of a wide surgical margin or a free margin. The width of the free margin depends on the type of the cancer, the method of removal (CCPDMA, Mohs surgery, POMA, etc.). The margin can be as little as 1 mm for basal cell cancer using CCPDMA or Mohs surgery, to several centimeters for aggressive cancers. The effectiveness of chemotherapy is often limited by toxicity to other tissues in the body. Radiation can also cause damage to normal tissue.
Because cancer is a class of diseases,[83][84] it is unlikely that there will ever be a single "cure for cancer" any more than there will be a single treatment for all infectious diseases.[85] Angiogenesis inhibitors were once thought to have potential as a "silver bullet" treatment applicable to many types of cancer, but this has not been the case in practice.[86]
Experimental cancer treatments are treatments that are being studied to see whether they work. Typically, these are studied in clinical trials to compare the proposed treatment to the best existing treatment. They may be entirely new treatments, or they may be treatments that have been used successfully in one type of cancer, and are now being tested to see whether they are effective in another type.[87] More and more, such treatments are being developed alongside companion diagnostic tests to target the right drugs to the right patients, based on their individual biology.[88]
Alternative treatments
Alternative cancer treatments are treatments used by alternative medicine practitioners. These are a group of non-related interventions that do not fit the rigors of Western medicine and include mind–body interventions, herbal preparations, massage, acupuncture, reiki, electrical stimulation devices, and a variety of strict dietary regimens among others.
Alternative cancer treatments have never been shown to be effective at killing cancer cells in research studies, but remain popular in some cultures and religions. Some are dangerous, but most are harmless or provide the patient with a degree of physical or emotional comfort. Alternative cancer treatment has also been a fertile field for hoaxes aimed at stripping desperate patients of their money.[89]
Many physicians are supportive of patients using alternative medicine in addition to standard management, especially for symptom management, though certain types of alternative herbs or diets could actually interfere with treatments and should be discussed with an oncologist if undergoing chemotherapy or radiation treatments.[90][91][92][93]
Palliative care
Palliative care is a multidisciplinary approach to symptom management that aims to reduce the physical, emotional, spiritual, and psycho-social distress experienced by people with cancer. Unlike treatment that is aimed at directly killing cancer cells, the primary goal of palliative care is to make the person feel better as soon as possible.
Palliative care is often confused with hospice and therefore only involved when patients approach end of life. Like hospice care, palliative care attempts to help the person cope with the immediate needs and to increase the person's comfort. Unlike hospice care, palliative care does not require patients to stop treatment aimed at prolonging their lives or curing the cancer.
Multiple national medical guidelines recommend early palliative care involvement in people whose cancer has produced complex symptoms (pain, shortness of breath, fatigue, nausea) or who need help coping with their illness. In people who have metastatic disease when first diagnosed, oncologists should consider a palliative care consult immediately. Additionally, an oncologist should consider a palliative care consult in any patient they feel has a prognosis of less than 12 months even if continuing aggressive treatment.[94][95][96]
Prognosis
See also: Cancer survivorCancer has a reputation as a deadly disease. Taken as a whole, about half of patients receiving treatment for invasive cancer (excluding carcinoma in situ and non-melanoma skin cancers) die from cancer or its treatment. However, the survival rates vary dramatically by type of cancer, with the range running from basically all patients surviving to almost no patients surviving.
Patients who receive a long-term remission or permanent cure may have physical and emotional complications from the disease and its treatment. Surgery may have amputated body parts or removed internal organs, or the cancer may have damaged delicate structures, like the part of the ear that is responsible for the sense of balance; in some cases, this requires extensive physical rehabilitation or occupational therapy so that the patient can walk or engage in other activities of daily living. Chemo brain is a usually short-term cognitive impairment associated with some treatments. Cancer-related fatigue usually resolves shortly after the end of treatment, but may be lifelong. Cancer-related pain may require ongoing treatment. Younger patients may be unable to have children. Some patients may be anxious or psychologically traumatized as a result of their experience of the diagnosis or treatment.
Survivors generally need to have regular medical screenings to ensure that the cancer has not returned, to manage any ongoing cancer-related conditions, and to screen for new cancers. Cancer survivors, even when permanently cured of the first cancer, have approximately double the normal risk of developing another primary cancer. Some advocates have promoted "survivor care plans"—written documents detailing the diagnosis, all previous treatment, and all recommended cancer screening and other care requirements for the future—as a way of organizing the extensive medical information that survivors and their future healthcare providers need.
Progressive and disseminated malignant disease harms the cancer patient's quality of life, and some cancer treatments, including common forms of chemotherapy, have severe side effects. In the advanced stages of cancer, many patients need extensive care, affecting family members and friends. Palliative care aims to improve the patient's immediate quality of life, regardless of whether further treatment is undertaken. Hospice programs assist patients similarly, especially when a terminally ill patient has rejected further treatment aimed at curing the cancer. Both styles of service offer home health nursing and respite care.
Predicting either short-term or long-term survival is difficult and depends on many factors. The most important factors are the particular kind of cancer and the patient's age and overall health. Medically frail patients with many comorbidities have lower survival rates than otherwise healthy patients. A centenarian is unlikely to survive for five years even if the treatment is successful. Patients who report a higher quality of life tend to survive longer.[97] People with lower quality of life may be affected by major depressive disorder and other complications from cancer treatment and/or disease progression that both impairs their quality of life and reduces their quantity of life. Additionally, patients with worse prognoses may be depressed or report a lower quality of life directly because they correctly perceive that their condition is likely to be fatal.
In the developed world, one in three people will be diagnosed with invasive cancer during their lifetimes. If all people with cancer survived and cancer occurred randomly, the lifetime odds of developing a second primary cancer would be one in nine.[98] However, cancer survivors have an increased risk of developing a second primary cancer, and the odds are about two in nine.[98] About half of these second primaries can be attributed to the normal one-in-nine risk associated with random chance.[98] The increased risk is believed to be primarily due to the same risk factors that produced the first cancer (such as the person's genetic profile, alcohol and tobacco use, obesity, and environmental exposures), and partly due to the treatment for the first cancer, which typically includes mutagenic chemotherapeutic drugs or radiation.[98] Cancer survivors may also be more likely to comply with recommended screening, and thus may be more likely than average to detect cancers.[98]
Despite strong social pressure to maintain an upbeat, optimistic attitude or act like a determined "fighter" to "win the battle", personality traits have no connection to survival.[99]
Epidemiology
Main article: Epidemiology of cancer Death rate from malignant cancer per 100,000 inhabitants in 2004.[100]
Death rate from malignant cancer per 100,000 inhabitants in 2004.[100] no data≤ 5555-8080-105105-130130-155155-180180-205205-230230-255255-280280-305≥ 305
no data≤ 5555-8080-105105-130130-155155-180180-205205-230230-255255-280280-305≥ 305In 2008 approximately 12.7 million cancers were diagnosed (excluding non-melanoma skin cancers and other non-invasive cancers) and 7.6 million people died of cancer worldwide.[3] Cancers as a group account for approximately 13% of all deaths each year with the most common being: lung cancer (1.3 million deaths), stomach cancer (803,000 deaths), colorectal cancer (639,000 deaths), liver cancer (610,000 deaths), and breast cancer (519,000 deaths).[101] This makes invasive cancer the leading cause of death in the developed world and the second leading cause of death in the developing world.[3] Over half of cases occur in the developing world.[3]
Global cancer rates have been increasing primarily due to an aging population and lifestyle changes in the developing world.[3] The most significant risk factor for developing cancer is old age.[102] Although it is possible for cancer to strike at any age, most people who are diagnosed with invasive cancer are over the age of 65.[102] According to cancer researcher Robert A. Weinberg, "If we lived long enough, sooner or later we all would get cancer."[103] Some of the association between aging and cancer is attributed to immunosenescence,[104] errors accumulated in DNA over a lifetime, and age-related changes in the endocrine system.[105]
Some slow-growing cancers are particularly common. Autopsy studies in Europe and Asia have shown that up to 36% of people have undiagnosed and apparently harmless thyroid cancer at the time of their deaths, and that 80% of men develop prostate cancer by age 80.[106][107] As these cancers, often very small, did not cause the person's death, identifying them would have represented overdiagnosis rather than useful medical care.
The three most common childhood cancers are leukemia (34%), brain tumors (23%), and lymphomas (12%).[108] Rates of childhood cancer have increased between 0.6% per year between 1975 to 2002 in the United States[109] and by 1.1% per year between 1978 and 1997 in Europe.[108]
History
Hippocrates (ca. 460 BC – ca. 370 BC) described several kinds of cancers, referring to them with the Greek word carcinos (crab or crayfish), among others.[110] This name comes from the appearance of the cut surface of a solid malignant tumour, with "the veins stretched on all sides as the animal the crab has its feet, whence it derives its name".[111] Since it was against Greek tradition to open the body, Hippocrates only described and made drawings of outwardly visible tumors on the skin, nose, and breasts. Treatment was based on the humor theory of four bodily fluids (black and yellow bile, blood, and phlegm). According to the patient's humor, treatment consisted of diet, blood-letting, and/or laxatives. Through the centuries it was discovered that cancer could occur anywhere in the body, but humor-theory based treatment remained popular until the 19th century with the discovery of cells.
 Engraving with two views of a Dutch woman who had a tumor removed from her neck in 1689.
Engraving with two views of a Dutch woman who had a tumor removed from her neck in 1689.
Celsus (ca. 25 BC - 50 AD) translated carcinos into the Latin cancer, also meaning crab. Galen (2nd century AD) called benign tumours oncos, Greek for swelling, reserving Hippocrates' carcinos for malignant tumours. He later added the suffix -oma, Greek for swelling, giving the name carcinoma.
The oldest known description and surgical treatment of cancer was discovered in Egypt and dates back to approximately 1600 BC. The Papyrus describes 8 cases of ulcers of the breast that were treated by cauterization, with a tool called "the fire drill." The writing says about the disease, "There is no treatment."[112]
In the 16th and 17th centuries, it became more acceptable for doctors to dissect bodies to discover the cause of death. The German professor Wilhelm Fabry believed that breast cancer was caused by a milk clot in a mammary duct. The Dutch professor Francois de la Boe Sylvius, a follower of Descartes, believed that all disease was the outcome of chemical processes, and that acidic lymph fluid was the cause of cancer. His contemporary Nicolaes Tulp believed that cancer was a poison that slowly spreads, and concluded that it was contagious.[113]
The first cause of cancer was identified by British surgeon Percivall Pott, who discovered in 1775 that cancer of the scrotum was a common disease among chimney sweeps. The work of other individual physicians led to various insights, but when physicians started working together they could make firmer conclusions.
With the widespread use of the microscope in the 18th century, it was discovered that the 'cancer poison' spread from the primary tumor through the lymph nodes to other sites ("metastasis"). This view of the disease was first formulated by the English surgeon Campbell De Morgan between 1871 and 1874.[114] The use of surgery to treat cancer had poor results due to problems with hygiene. The renowned Scottish surgeon Alexander Monro saw only 2 breast tumor patients out of 60 surviving surgery for two years. In the 19th century, asepsis improved surgical hygiene and as the survival statistics went up, surgical removal of the tumor became the primary treatment for cancer. With the exception of William Coley who in the late 19th century felt that the rate of cure after surgery had been higher before asepsis (and who injected bacteria into tumors with mixed results), cancer treatment became dependent on the individual art of the surgeon at removing a tumor. During the same period, the idea that the body was made up of various tissues, that in turn were made up of millions of cells, laid rest the humor-theories about chemical imbalances in the body. The age of cellular pathology was born.
The genetic basis of cancer was recognised in 1902 by the German zoologist Theodor Boveri, professor of zoology at Munich and later in Würzburg.[115] He discovered a method to generate cells with multiple copies of the centrosome, a structure he discovered and named. He postulated that chromosomes were distinct and transmitted different inheritance factors. He suggested that mutations of the chromosomes could generate a cell with unlimited growth potential which could be passed onto its descendants. He proposed the existence of cell cycle check points, tumour suppressor genes and oncogenes. He speculated that cancers might be caused or promoted by radiation, physical or chemical insults or by pathogenic microorganisms.
 1938 poster identifying surgery, x-rays and radium as the proper treatments for cancer.
1938 poster identifying surgery, x-rays and radium as the proper treatments for cancer.
When Marie Curie and Pierre Curie discovered radiation at the end of the 19th century, they stumbled upon the first effective non-surgical cancer treatment. With radiation also came the first signs of multi-disciplinary approaches to cancer treatment. The surgeon was no longer operating in isolation, but worked together with hospital radiologists to help patients. The complications in communication this brought, along with the necessity of the patient's treatment in a hospital facility rather than at home, also created a parallel process of compiling patient data into hospital files, which in turn led to the first statistical patient studies.
A founding paper of cancer epidemiology was the work of Janet Lane-Claypon, who published a comparative study in 1926 of 500 breast cancer cases and 500 control patients of the same background and lifestyle for the British Ministry of Health. Her ground-breaking work on cancer epidemiology was carried on by Richard Doll and Austin Bradford Hill, who published "Lung Cancer and Other Causes of Death In Relation to Smoking. A Second Report on the Mortality of British Doctors" followed in 1956 (otherwise known as the British doctors study). Richard Doll left the London Medical Research Center (MRC), to start the Oxford unit for Cancer epidemiology in 1968. With the use of computers, the unit was the first to compile large amounts of cancer data. Modern epidemiological methods are closely linked to current[when?] concepts of disease and public health policy. Over the past 50 years, great efforts have been spent on gathering data across medical practise, hospital, provincial, state, and even country boundaries to study the interdependence of environmental and cultural factors on cancer incidence.
Cancer patient treatment and studies were restricted to individual physicians' practices until World War II, when medical research centers discovered that there were large international differences in disease incidence. This insight drove national public health bodies to make it possible to compile health data across practises and hospitals, a process that many countries do today. The Japanese medical community observed that the bone marrow of victims of the atomic bombings of Hiroshima and Nagasaki was completely destroyed. They concluded that diseased bone marrow could also be destroyed with radiation, and this led to the discovery of bone marrow transplants for leukemia. Since World War II, trends in cancer treatment are to improve on a micro-level the existing treatment methods, standardize them, and globalize them to find cures through epidemiology and international partnerships.
Society and culture
While many diseases (such as heart failure) may have a worse prognosis than most cases of cancer, it is the subject of widespread fear and taboos. Euphemisms, once "a long illness", and now informally as "the big C", provide distance and soothe superstitions.[116] This deep belief that cancer is necessarily a difficult and usually deadly disease is reflected in the systems chosen by society to compile cancer statistics: the most common form of cancer—non-melanoma skin cancers, accounting for about one-third of all cancer cases worldwide, but very few deaths[117][118]—are excluded from cancer statistics specifically because they are easily treated and almost always cured, often in a single, short, outpatient procedure.[119]
Cancer is regarded as a disease that must be "fought" to end the "civil insurrection"; a War on Cancer has been declared. Military metaphors are particularly common in descriptions of cancer's human effects, and they emphasize both the parlous state of the affected individual's health and the need for the individual to take immediate, decisive actions himself, rather than to delay, to ignore, or to rely entirely on others caring for him. The military metaphors also help rationalize radical, destructive treatments.[120][121]
In the 1970s, a relatively popular alternative cancer treatment was a specialized form of talk therapy, based on the idea that cancer was caused by a bad attitude.[89] People with a "cancer personality"—depressed, repressed, self-loathing, and afraid to express their emotions—were believed to have manifested cancer through subconscious desire. Some psychotherapists said that treatment to change the patient's outlook on life would cure the cancer.[89] Among other effects, this belief allows society to blame the victim for having caused the cancer (by "wanting" it) or having prevented its cure (by not becoming a sufficiently happy, fearless, and loving person).[122] It also increases patients' anxiety, as they incorrectly believe that natural emotions of sadness, anger or fear shorten their lives.[122] The idea was excoriated by the notoriously outspoken Susan Sontag, who published Illness as Metaphor while recovering from treatment for breast cancer in 1978.[89] Although the original idea is now generally regarded as nonsense, the idea partly persists in a reduced form with a widespread, but incorrect, belief that deliberately cultivating a habit of positive thinking will increase survival.[122] This notion is particularly strong in breast cancer culture.[122]
Research
Main article: Cancer researchCancer research is the intense scientific effort to understand disease processes and discover possible therapies.
Research about cancer causes focuses on the following issues:
- Agents (e.g. viruses) and events (e.g. mutations) which cause or facilitate genetic changes in cells destined to become cancer.
- The precise nature of the genetic damage, and the genes which are affected by it.
- The consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell, and in facilitating additional genetic events which lead to further progression of the cancer.
The improved understanding of molecular biology and cellular biology due to cancer research has led to a number of new, effective treatments for cancer since President Nixon declared "War on Cancer" in 1971. Since 1971 the United States has invested over $200 billion on cancer research; that total includes money invested by public and private sectors and foundations.[123] Despite this substantial investment, the country has seen a five percent decrease in the cancer death rate (adjusting for size and age of the population) between 1950 and 2005.[124]
Leading cancer research organizations and projects include the American Association for Cancer Research, the American Cancer Society (ACS), the American Society of Clinical Oncology, the European Organisation for Research and Treatment of Cancer, Cancer Research UK, ECCO - the European Cancer Organisation, the National Cancer Institute, the National Comprehensive Cancer Network, The Cancer Genome Atlas project at the NCI, and Translational Genomics Institute (TGen,TD2).
In pregnancy
Because cancer is largely a disease of older adults, it is not common in pregnant women. Cancer affects approximately 1 in 1,000 pregnant women.[125] The most common cancers found during pregnancy are the same as the most common cancers found in non-pregnant women during childbearing ages: breast cancer, cervical cancer, leukemia, lymphoma, melanoma, ovarian cancer, and colorectal cancer.[125]
Diagnosing a new cancer in a pregnant woman is difficult, in part because any symptoms are commonly assumed to be a normal discomfort associated with pregnancy.[125] As a result, cancer is typically discovered at a somewhat later stage than average in many pregnant or recently pregnant women. Some imaging procedures, such as MRIs (magnetic resonance imaging), CT scans, ultrasounds, and mammograms with fetal shielding are considered safe during pregnancy; some others, such as PET scans are not.[125]
Treatment is generally the same as for non-pregnant women.[125] However, radiation and radioactive drugs are normally avoided during pregnancy, especially if the fetal dose might exceed 100 cGy. In some cases, some or all treatments are postponed until after birth if the cancer is diagnosed late in the pregnancy. Early deliveries to speed the start of treatment are not uncommon. Surgery is generally safe, but pelvic surgeries during the first trimester may cause miscarriage. Some treatments, especially certain chemotherapy drugs given during the first trimester, increase the risk of birth defects and pregnancy loss (spontaneous abortions and stillbirths).[125]
Elective abortions are not required and, for the most common forms and stages of cancer, do not improve the likelihood of the mother surviving or being cured.[125] In a few instances, such as advanced uterine cancer, the pregnancy cannot be continued, and in others, such as an acute leukemia discovered early in pregnancy, the pregnant woman may choose to have abortion so that she can begin aggressive chemotherapy without worrying about birth defects.[125]
Some treatments may interfere with the mother's ability to give birth vaginally or to breastfeed her baby.[125] Cervical cancer may require birth by Caesarean section. Radiation to the breast reduces the ability of that breast to produce milk and increases the risk of mastitis. Also, when chemotherapy is being given after birth, many of the drugs pass through breast milk to the baby, which could harm the baby.[125]
Notes
- ^ a b c d e f g Anand P, Kunnumakkara AB, Kunnumakara AB, et al. (September 2008). "Cancer is a Preventable Disease that Requires Major Lifestyle Changes". Pharm. Res. 25 (9): 2097–116. doi:10.1007/s11095-008-9661-9. PMC 2515569. PMID 18626751. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2515569.
- ^ Kinzler, Kenneth W.; Vogelstein, Bert (2002). "Introduction". The genetic basis of human cancer (2nd, illustrated, revised ed.). New York: McGraw-Hill, Medical Pub. Division. p. 5. ISBN 978-0-07-137050-9. http://books.google.co.uk/books?id=pYG09OPbXp0C&pg=PA5.
- ^ a b c d e f Jemal, A; Bray, F, Center, MM, Ferlay, J, Ward, E, Forman, D (2011-02-04). "Global cancer statistics". CA: a cancer journal for clinicians 61 (2): 69–90. doi:10.3322/caac.20107. PMID 21296855.
- ^ NIH
- ^ a b Sasco AJ, Secretan MB, Straif K (August 2004). "Tobacco smoking and cancer: a brief review of recent epidemiological evidence". Lung cancer (Amsterdam, Netherlands) 45 Suppl 2: S3–9. doi:10.1016/j.lungcan.2004.07.998. PMID 15552776.
- ^ Biesalski HK, Bueno de Mesquita B, Chesson A, et al. (1998). "European Consensus Statement on Lung Cancer: risk factors and prevention. Lung Cancer Panel". CA: a cancer journal for clinicians 48 (3): 167–76; discussion 164–6. doi:10.3322/canjclin.48.3.167. PMID 9594919. http://caonline.amcancersoc.org/cgi/reprint/48/3/167.pdf.
- ^ Seitz HK, Pöschl G, Simanowski UA (1998). "Alcohol and cancer". Recent developments in alcoholism : an official publication of the American Medical Society on Alcoholism, the Research Society on Alcoholism, and the National Council on Alcoholism 14: 67–95. PMID 9751943.
- ^ Schütze, M; Boeing, H, Pischon, T, Rehm, J, Kehoe, T, Gmel, G, Olsen, A, Tjønneland, AM, Dahm, CC, Overvad, K, Clavel-Chapelon, F, Boutron-Ruault, MC, Trichopoulou, A, Benetou, V, Zylis, D, Kaaks, R, Rohrmann, S, Palli, D, Berrino, F, Tumino, R, Vineis, P, Rodríguez, L, Agudo, A, Sánchez, MJ, Dorronsoro, M, Chirlaque, MD, Barricarte, A, Peeters, PH, van Gils, CH, Khaw, KT, Wareham, N, Allen, NE, Key, TJ, Boffetta, P, Slimani, N, Jenab, M, Romaguera, D, Wark, PA, Riboli, E, Bergmann, MM (2011-04-07). "Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study". BMJ (Clinical research ed.) 342: d1584. doi:10.1136/bmj.d1584. PMC 3072472. PMID 21474525. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3072472.
- ^ Kuper H, Boffetta P, Adami HO (September 2002). "Tobacco use and cancer causation: association by tumour type". Journal of internal medicine 252 (3): 206–24. doi:10.1046/j.1365-2796.2002.01022.x. PMID 12270001.
- ^ a b Kuper H, Adami HO, Boffetta P (June 2002). "Tobacco use, cancer causation and public health impact". Journal of internal medicine 251 (6): 455–66. doi:10.1046/j.1365-2796.2002.00993.x. PMID 12028500.
- ^ Proctor RN (May 2004). "The global smoking epidemic: a history and status report". Clinical lung cancer 5 (6): 371–6. doi:10.3816/CLC.2004.n.016. PMID 15217537. http://cigjournals.metapress.com/content/f515k445g2218ht7/fulltext.pdf.
- ^ Irigaray P, Newby JA, Clapp R, et al. (December 2007). "Lifestyle-related factors and environmental agents causing cancer: an overview". Biomed. Pharmacother. 61 (10): 640–58. doi:10.1016/j.biopha.2007.10.006. PMID 18055160.
- ^ a b c "WHO calls for prevention of cancer through healthy workplaces" (Press release). World Health Organization. 2007-04-27. http://www.who.int/mediacentre/news/notes/2007/np19/en/index.html. Retrieved 2007-10-13.
- ^ "National Institute for Occupational Safety and Health- Occupational Cancer". United States National Institute for Occupational Safety and Health. http://www.cdc.gov/niosh/topics/cancer/. Retrieved 2007-10-13.
- ^ a b c d Kushi LH, Byers T, Doyle C, et al. (2006). "American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity". CA Cancer J Clin 56 (5): 254–81. doi:10.3322/canjclin.56.5.254. PMID 17005596. http://caonline.amcancersoc.org/cgi/reprint/56/5/254.pdf.
- ^ Park, S; Bae, J, Nam, BH, Yoo, KY (2008 Jul-Sep). "Aetiology of cancer in Asia" (PDF). Asian Pacific journal of cancer prevention 9 (3): 371–80. PMID 18990005. http://www.apocpcontrol.org/page/popup_paper_file_view.php?pno=MzcxIFBhcmsucCZrY29kZT04MjI=&pgubun=i.
- ^ Brenner, H; Rothenbacher, D, Arndt, V (2009). "Epidemiology of stomach cancer". Methods in molecular biology (Clifton, N.J.). Methods in Molecular Biology 472: 467–77. doi:10.1007/978-1-60327-492-0_23. ISBN 978-1-60327-491-3. PMID 19107449.
- ^ Buell P, Dunn JE (1965). "Cancer mortality among Japanese Issei and Nisei of California". Cancer 18 (5): 656–64. doi:10.1002/1097-0142(196505)18:5<656::AID-CNCR2820180515>3.0.CO;2-3. PMID 14278899.
- ^ Pagano JS, Blaser M, Buendia MA, et al. (December 2004). "Infectious agents and cancer: criteria for a causal relation". Semin. Cancer Biol. 14 (6): 453–71. doi:10.1016/j.semcancer.2004.06.009. PMID 15489139.
- ^ Samaras, Vassilis; Rafailidis, Petros I.; Mourtzoukou, Eleni G.; Peppas, George; Falagas, Matthew E. (May 2010). "Chronic bacterial and parasitic infections and cancer: a review" (PDF). The Journal of Infection in Developing Countries 4 (5): 267–281. ISSN 1972-2680. PMID 20539059. http://www.jidc.org/index.php/journal/article/download/20539059/387.
- ^ a b c d e f g h i j k l Little, John B (2000). "Chapter 14: Ionizing Radiation". In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20793/. Retrieved 31 January 2011.
- ^ Berrington de González A, Mahesh M, Kim KP, et al. (December 2009). "Projected cancer risks from computed tomographic scans performed in the United States in 2007". Arch. Intern. Med. 169 (22): 2071–7. doi:10.1001/archinternmed.2009.440. PMID 20008689. http://archinte.ama-assn.org/cgi/reprint/169/22/2071.pdf.
- ^ Brenner DJ, Hall EJ (November 2007). "Computed tomography--an increasing source of radiation exposure" (PDF). N. Engl. J. Med. 357 (22): 2277–84. doi:10.1056/NEJMra072149. PMID 18046031. http://www.nejm.org/doi/pdf/10.1056/NEJMra072149.
- ^ a b Cleaver, James E and David L Mitchell (2000). "15. Ultraviolet Radiation Carcinogenesis". In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20854/. Retrieved 31 January 2011.
- ^ "IARC classifies radiofrequency electromagnetic fields as possibly carcinogenic to humans". World Health Organization. http://www.iarc.fr/en/media-centre/pr/2011/pdfs/pr208_E.pdf.
- ^ a b c Roukos, DH (2009 Apr). "Genome-wide association studies: how predictable is a person's cancer risk?" (PDF). Expert review of anticancer therapy 9 (4): 389–92. doi:10.1586/era.09.12. PMID 19374592. http://www.expert-reviews.com/doi/pdfplus/10.1586/era.09.12.
- ^ a b c d e Maltoni, Cesare Franco Minardi, and James F Holland (2000). "Chapter 16: Physical Carcinogens". In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20770/. Retrieved 31 January 2011.
- ^ a b c d e f g Gaeta, John F (2000). "Chapter 17: Trauma and Inflammation". In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20784/. Retrieved 27 January 2011.
- ^ a b c d e f g h i j k Henderson, Brian E, Leslie Bernstein, and Ronald K Ross (2000). "Chapter 13: Hormones and the Etiology of Cancer". In Bast RC, Kufe DW, Pollock RE, et al.. Holland-Frei Cancer Medicine (5th ed.). Hamilton, Ontario: B.C. Decker. ISBN 1-55009-113-1. http://www.ncbi.nlm.nih.gov/books/NBK20759/. Retrieved 27 January 2011.
- ^ a b Tolar J, Neglia JP (June 2003). "Transplacental and other routes of cancer transmission between individuals". J Pediatr Hematol Oncol. 25 (6): 430–4. doi:10.1097/00043426-200306000-00002. PMID 12794519. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1077-4114&volume=25&issue=6&spage=430.
- ^ Dingli D, Nowak MA (September 2006). "Infectious Cancer Cells". Nature 443 (7107): 35–6. Bibcode 2006Natur.443...35D. doi:10.1038/443035a. PMC 2711443. PMID 16957717. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2711443.
- ^ "Cancer Spread By Transplantation Extremely Rare: In Very Rare Case, Woman Develops Leukemia from Liver Transplant". http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Cancer_Spread_By_Transplantation_Extremely_Rare.asp.[dead link]
- ^ "The Nobel Prize in Physiology or Medicine 1980". http://nobelprize.org/nobel_prizes/medicine/laureates/1980/presentation-speech.html.
- ^ Murgia C, Pritchard JK, Kim SY, Fassati A, Weiss RA (2006). "Clonal Origin and Evolution of a Transmissible Cancer". Cell 126 (3): 477–87. doi:10.1016/j.cell.2006.05.051. PMC 2593932. PMID 16901782. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2593932.
- ^ Croce CM (January 2008). "Oncogenes and cancer" (PDF). The New England journal of medicine 358 (5): 502–11. doi:10.1056/NEJMra072367. PMID 18234754. http://www.nejm.org/doi/pdf/10.1056/NEJMra072367.
- ^ Knudson AG (November 2001). "Two genetic hits (more or less) to cancer". Nature reviews. Cancer 1 (2): 157–62. doi:10.1038/35101031. PMID 11905807.
- ^ Nelson DA, Tan TT, Rabson AB, Anderson D, Degenhardt K, White E (September 2004). "Hypoxia and defective apoptosis drive genomic instability and tumorigenesis". Genes & Development 18 (17): 2095–107. doi:10.1101/gad.1204904. PMC 515288. PMID 15314031. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=515288.
- ^ Merlo LM, Pepper JW, Reid BJ, Maley CC (December 2006). "Cancer as an evolutionary and ecological process". Nat. Rev. Cancer 6 (12): 924–35. doi:10.1038/nrc2013. PMID 17109012.
- ^ "Cancer prevention: 7 steps to reduce your risk". Mayo Clinic. 2008-09-27. http://www.mayoclinic.com/health/cancer-prevention/CA00024. Retrieved 2010-01-30.
- ^ Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M (2005). "Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors". Lancet 366 (9499): 1784–93. doi:10.1016/S0140-6736(05)67725-2. PMID 16298215.
- ^ "Cancer". World Health Organization. http://www.who.int/mediacentre/factsheets/fs297/en/. Retrieved 2011-01-09.
- ^ "Recommendations". dietandcancerreport.org. Retrieved on 27 August 2008.
- ^ Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Chapter 12 World Cancer Research Fund (2007). ISBN 978-0-9722522-2-5.
- ^ Slattery ML, Boucher KM, Caan BJ, Potter JD, Ma KN (1998). "Eating patterns and risk of colon cancer". Am. J. Epidemiol. 148 (1): 4–16. PMID 9663397.
- ^ Larsson SC, Wolk A (2007). "Coffee consumption and risk of liver cancer: a meta-analysis". Gastroenterology 132 (5): 1740–5. doi:10.1053/j.gastro.2007.03.044. PMID 17484871.
- ^ Ward MH, Sinha R, Heineman EF, et al. (1997). "Risk of adenocarcinoma of the stomach and esophagus with meat cooking method and doneness preference". Int. J. Cancer 71 (1): 14–9. doi:10.1002/(SICI)1097-0215(19970328)71:1<14::AID-IJC4>3.0.CO;2-6. PMID 9096659.
- ^ Sinha R, Peters U, Cross AJ, et al. (2005). "Meat, meat cooking methods and preservation, and risk for colorectal adenoma". Cancer Res. 65 (17): 8034–41. doi:10.1158/0008-5472.CAN-04-3429 (inactive 2010-01-06). PMID 16140978. http://cancerres.aacrjournals.org/content/65/17/8034.full.pdf.
- ^ Steck SE, Gaudet MM, Eng SM, et al. (2007). "Cooked meat and risk of breast cancer--lifetime versus recent dietary intake". Epidemiology (Cambridge, Mass.) 18 (3): 373–82. doi:10.1097/01.ede.0000259968.11151.06. PMID 17435448.
- ^ Anderson KE, Kadlubar FF, Kulldorff M, et al. (2005). "Dietary intake of heterocyclic amines and benzo(a)pyrene: associations with pancreatic cancer". Cancer Epidemiol. Biomarkers Prev. 14 (9): 2261–5. doi:10.1158/1055-9965.EPI-04-0514. PMID 16172241.
- ^ Zheng W, Lee SA (2009). "Well-done Meat Intake, Heterocyclic Amine Exposure, and Cancer Risk". Nutr Cancer. 61 (4): 437–46. doi:10.1080/01635580802710741. PMC 2769029. PMID 19838915. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2769029.
- ^ Boffetta P, Couto E, Wichmann J, et al. (2010). "Fruit and vegetable intake and overall cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC)". J Natl Cancer Inst 8 (102): 529–37. doi:10.1093/jnci/djq072. PMID 20371762.
- ^ Ornish D et al. (2005). "Intensive lifestyle changes may affect the progression of prostate cancer". The Journal of Urology 174 (3): 1065–9; discussion 1069–70. doi:10.1097/01.ju.0000169487.49018.73. PMID 16094059.
- ^ Chlebowski RT, Blackburn GL, Thomson CA, et al. (2006). "Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study". J. Natl. Cancer Inst. 98 (24): 1767–76. doi:10.1093/jnci/djj494. PMID 17179478.
- ^ Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW (January 2011). "Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials". Lancet 377 (9759): 31–41. doi:10.1016/S0140-6736(10)62110-1. PMID 21144578.
- ^ Vogel V, Costantino J, Wickerham D, Cronin W, Cecchini R, Atkins J, Bevers T, Fehrenbacher L, Pajon E, Wade J, Robidoux A, Margolese R, James J, Lippman S, Runowicz C, Ganz P, Reis S, McCaskill-Stevens W, Ford L, Jordan V, Wolmark N (2006). "Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial". JAMA 295 (23): 2727–41. doi:10.1001/jama.295.23.joc60074. PMID 16754727.
- ^ Thompson I, Goodman P, Tangen C, Lucia M, Miller G, Ford L, Lieber M, Cespedes R, Atkins J, Lippman S, Carlin S, Ryan A, Szczepanek C, Crowley J, Coltman C (2003). "The influence of finasteride on the development of prostate cancer". N Engl J Med 349 (3): 215–24. doi:10.1056/NEJMoa030660. PMID 12824459.
- ^ Hallak A, Alon-Baron L, Shamir R, Moshkowitz M, Bulvik B, Brazowski E, Halpern Z, Arber N (2003). "Rofecoxib reduces polyp recurrence in familial polyposis". Dig Dis Sci 48 (10): 1998–2002. doi:10.1023/A:1026130623186. PMID 14627347.
- ^ Baron J, Sandler R, Bresalier R, Quan H, Riddell R, Lanas A, Bolognese J, Oxenius B, Horgan K, Loftus S, Morton D (2006). "A randomized trial of rofecoxib for the chemoprevention of colorectal adenomas". Gastroenterology 131 (6): 1674–82. doi:10.1053/j.gastro.2006.08.079. PMID 17087947.
- ^ Bertagnolli M, Eagle C, Zauber A, Redston M, Solomon S, Kim K, Tang J, Rosenstein R, Wittes J, Corle D, Hess T, Woloj G, Boisserie F, Anderson W, Viner J, Bagheri D, Burn J, Chung D, Dewar T, Foley T, Hoffman N, Macrae F, Pruitt R, Saltzman J, Salzberg B, Sylwestrowicz T, Gordon G, Hawk E (2006). "Celecoxib for the prevention of sporadic colorectal adenomas". N Engl J Med 355 (9): 873–84. doi:10.1056/NEJMoa061355. PMID 16943400.
- ^ "Vitamins and minerals: not for cancer or cardiovascular prevention". Prescrire Int 19 (108): 182. August 2010. PMID 20939459.
- ^ Giovannucci E, Liu Y, Rimm EB, et al. (April 2006). "Prospective study of predictors of vitamin D status and cancer incidence and mortality in men". J. Natl. Cancer Inst. 98 (7): 451–9. doi:10.1093/jnci/djj101. PMID 16595781.
- ^ "Vitamin D Has Role in Colon Cancer Prevention". Archived from the original on December 4, 2006. http://web.archive.org/web/20061204052746/http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Vitamin_D_Has_Role_in_Colon_Cancer_Prevention.asp. Retrieved 2007-07-27.
- ^ Schwartz GG, Blot WJ (April 2006). "Vitamin D status and cancer incidence and mortality: something new under the sun". J. Natl. Cancer Inst. 98 (7): 428–30. doi:10.1093/jnci/djj127. PMID 16595770. http://jnci.oxfordjournals.org/content/98/7/428.full.pdf.
- ^ "Questions and answers about beta carotene chemoprevention trials". National Cancer Institute. 1997-06-27. http://www.cancer.gov/PDF/FactSheet/fs4_13.pdf. Retrieved 2009-04-23.
- ^ Cole BF, Baron JA, Sandler RS, et al. (2007). "Folic acid for the prevention of colorectal adenomas: a randomized clinical trial". Journal of the American Medical Association 297 (21): 2351–9. doi:10.1001/jama.297.21.2351. PMID 17551129. http://jama.ama-assn.org/content/297/21/2351.full.pdf.
- ^ a b c "Cancer Vaccine Fact Sheet". NCI. 2006-06-08. http://www.cancer.gov/cancertopics/factsheet/cancervaccine. Retrieved 2008-11-15.
- ^ a b c "What Is Cancer Screening?". National Cancer Institute. http://www.cancer.gov/cancertopics/pdq/screening/overview/Patient.
- ^ a b c d Wilson JMG, Jungner G. (1968) Principles and practice of screening for disease. Geneva:World Health Organization. Public Health Papers, #34.
- ^ "Screening for Cervical Cancer". U.S. Preventive Services Task Force. 2003. http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm.
- ^ "Screening for Colorectal Cancer". U.S. Preventive Services Task Force. 2008. http://www.uspreventiveservicestaskforce.org/uspstf/uspscolo.htm.
- ^ "Screening for Skin Cancer". U.S. Preventive Services Task Force. 2009. http://www.uspreventiveservicestaskforce.org/uspstf/uspsskca.htm.
- ^ "Screening for Oral Cancer". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspsoral.htm.
- ^ "Lung Cancer Screening". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspslung.htm.
- ^ "Screening for Prostate Cancer". U.S. Preventive Services Task Force. 2008. http://www.uspreventiveservicestaskforce.org/uspstf/uspsprca.htm.
- ^ "Screening for Bladder Cancer". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm.
- ^ "Screening for Testicular Cancer". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm.
- ^ "Screening for Ovarian Cancer". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspsovar.htm.
- ^ "Screening for Pancreatic Cancer". U.S. Preventive Services Task Force. 2004. http://www.uspreventiveservicestaskforce.org/uspstf/uspspanc.htm.
- ^ Chou, MD, Roger; Croswell, MD, MPH, Jennifer M.; Dana, MLS, Tracy; Bougatous, BS, Christina; Blazina, MPH, Ian; Fu, PhD, Rongwei; Gleitsmann, MD, MPH, Ken; Koenig, MD, MPH, Helen C. et al. (7 October 2011). "Screening for Prostate Cancer - A Review of the Evidence for the U.S. Preventive Services Task Force". United States Preventive Services Task Force. http://www.uspreventiveservicestaskforce.org/uspstf12/prostate/prostateart.htm. Retrieved 2011-10-08.
- ^ "Screening for Breast Cancer". U.S. Preventive Services Task Force. 2009. http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm.
- ^ Gøtzsche PC, Nielsen M (2009). Gøtzsche, Peter C. ed. "Screening for breast cancer with mammography". Cochrane Database Syst Rev (4): CD001877. doi:10.1002/14651858.CD001877.pub3. PMID 19821284.
- ^ a b Gulati, AP; Domchek, SM (2008 Jan). "The clinical management of BRCA1 and BRCA2 mutation carriers". Current oncology reports 10 (1): 47–53. doi:10.1007/s11912-008-0008-9. PMID 18366960.
- ^ "What Is Cancer?". National Cancer Institute. http://www.cancer.gov/cancertopics/what-is-cancer. Retrieved 2009-08-17.
- ^ "Cancer Fact Sheet". Agency for Toxic Substances & Disease Registry. 2002-08-30. http://www.atsdr.cdc.gov/COM/cancer-fs.html. Retrieved 2009-08-17.
- ^ Wanjek, Christopher (2006-09-16). "Exciting New Cancer Treatments Emerge Amid Persistent Myths". http://www.livescience.com/health/060919_bad_cancer.html. Retrieved 2009-08-17.
- ^ Hayden, Erika C. (2009-04-08). "Cutting off cancer's supply lines". Nature 458 (7239): 686–687. doi:10.1038/458686b. PMID 19360048.
- ^ Sleigh SH, Barton CL (2010). "Repurposing Strategies for Therapeutics". Pharm Med 24 (3): 151–159. doi:10.2165/11536770-000000000-00000. http://adisonline.com/pharmaceuticalmedicine/Fulltext/2010/24030/Repurposing_Strategies_for_Therapeutics.4.aspx.
- ^ Winther H, Jorgensen JT (2010). "Drug-Diagnostic Co-Development in Cancer". Pharm Med 24 (6): 363–375. doi:10.2165/11586320-000000000-00000. http://adisonline.com/pharmaceuticalmedicine/Fulltext/2010/24060/Drug_Diagnostic_Co_Development_in_Cancer.5.aspx.
- ^ a b c d Olson, James Stuart (2002). Bathsheba's Breast: Women, Cancer and History. Baltimore: The Johns Hopkins University Press. pp. 145–170. ISBN 0-8018-6936-6. OCLC 186453370.
- ^ Astin, JA; Marie, A, Pelletier, KR, Hansen, E, Haskell, WL (1998-11-23). "A review of the incorporation of complementary and alternative medicine by mainstream physicians". Archives of internal medicine 158 (21): 2303–10. doi:10.1001/archinte.158.21.2303. PMID 9827781.
- ^ Lawenda, BD; Kelly, KM, Ladas, EJ, Sagar, SM, Vickers, A, Blumberg, JB (2008-06-04). "Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy?". Journal of the National Cancer Institute 100 (11): 773–83. doi:10.1093/jnci/djn148. PMID 18505970.
- ^ Richardson, MA; Mâsse, LC, Nanny, K, Sanders, C (2004 Nov). "Discrepant views of oncologists and cancer patients on complementary/alternative medicine". Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer 12 (11): 797–804. doi:10.1007/s00520-004-0677-3. PMID 15378417.
- ^ Brumley, R; Enguidanos, S, Jamison, P, Seitz, R, Morgenstern, N, Saito, S, McIlwane, J, Hillary, K, Gonzalez, J (2007 Jul). "Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care". Journal of the American Geriatrics Society 55 (7): 993–1000. doi:10.1111/j.1532-5415.2007.01234.x. PMID 17608870.
- ^ "NCCN Guidelines". http://www.nccn.org/professionals/physician_gls/default.asp.
- ^ "Clinical Practice Guidelines for Quality Palliative Care". The National Consensus Project for Quality Palliative Care (NCP). http://www.nationalconsensusproject.org/guideline.pdf.
- ^ Levy, MH; Back, A, Bazargan, S, Benedetti, C, Billings, JA, Block, S, Bruera, E, Carducci, MA, Dy, S, Eberle, C, Foley, KM, Harris, JD, Knight, SJ, Milch, R, Rhiner, M, Slatkin, NE, Spiegel, D, Sutton, L, Urba, S, Von Roenn, JH, Weinstein, SM, National Comprehensive Cancer Network (September 2006). "Palliative care. Clinical practice guidelines in oncology". Journal of the National Comprehensive Cancer Network: JNCCN 4 (8): 776–818. PMID 16948956.
- ^ Montazeri A (2009-12-23). "Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008". Health Qual Life Outcomes 7: 102. doi:10.1186/1477-7525-7-102. PMC 2805623. PMID 20030832. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2805623.
- ^ a b c d e Rheingold, Susan; Neugut, Alfred; Meadows, Anna (2003). "156: Secondary Cancers: Incidence, Risk Factors, and Management". In Frei, Emil; Kufe, Donald W.; Holland, James F.. Holland-Frei Cancer Medicine (6th ed.). Hamilton, Ont: BC Decker. p. 2399. ISBN 1-55009-213-8. http://www.ncbi.nlm.nih.gov/books/NBK20948/. Retrieved 5 November 2009.
- ^ Nakaya N, Bidstrup PE, Saito-Nakaya K, et al. (August 2010). "Personality traits and cancer risk and survival based on Finnish and Swedish registry data". Am. J. Epidemiol. 172 (4): 377–85. doi:10.1093/aje/kwq046. PMID 20639285. Lay summary – The New York Times (25 January 2011).
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
- ^ WHO (February 2006). "Cancer". World Health Organization. http://www.who.int/mediacentre/factsheets/fs297/en/. Retrieved 2011-01-05.
- ^ a b Coleman, William B. and Rubinas, Tara C. (2009). "4". In Tsongalis, Gregory J. and Coleman, William L.. Molecular Pathology: The Molecular Basis of Human Disease. Amsterdam: Elsevier Academic Press. pp. 66. ISBN 0-12-374419-9.
- ^ Johnson, George (28 December 2010). "Unearthing Prehistoric Tumors, and Debate". The New York Times. http://www.nytimes.com/2010/12/28/health/28cancer.html.
- ^ Pawelec, G; Derhovanessian, E, Larbi, A (2010 Aug). "Immunosenescence and cancer". Critical reviews in oncology/hematology 75 (2): 165–72. doi:10.1016/j.critrevonc.2010.06.012. PMID 20656212.
- ^ Anisimov, VN; Sikora, E, Pawelec, G (2009 Aug). "Relationships between cancer and aging: a multilevel approach". Biogerontology 10 (4): 323–38. doi:10.1007/s10522-008-9209-8. PMID 19156531.
- ^ Fraumeni, Joseph F.; Schottenfeld, David; Marshall, James M. (2006). Cancer epidemiology and prevention. Oxford [Oxfordshire]: Oxford University Press. pp. 977. ISBN 0-19-514961-0.
- ^ Bostwick, David G.; Eble, John N. (2007). Urological Surgical Pathology. St. Louis: Mosby. p. 468. ISBN 0-323-01970-6.
- ^ a b Kaatsch, P (2010 Jun). "Epidemiology of childhood cancer". Cancer treatment reviews 36 (4): 277–85. doi:10.1016/j.ctrv.2010.02.003. PMID 20231056.
- ^ Ward, EM; Thun, MJ, Hannan, LM, Jemal, A (2006 Sep). "Interpreting cancer trends". Annals of the New York Academy of Sciences 1076: 29–53. Bibcode 2006NYASA1076...29W. doi:10.1196/annals.1371.048. PMID 17119192.
- ^ "The History of Cancer. Institut Jules Bordet (Association Hospitalière de Bruxelles - Centre des Tumeurs de ULB). Retrieved 2010-11-19". Bordet.be. http://www.bordet.be/en/presentation/history/cancer_e/cancer1.htm. Retrieved 2011-01-29.
- ^ Moss, Ralph W. (2004). "Galen on Cancer". CancerDecisions. http://www.cancerdecisions.com/speeches/galen1989.html. Moss in turn attributes this reason for the name to Paul of Aegina, 7th Century AD, quoted in Michael Shimkin, Contrary to Nature, Washington, D.C.: Superintendent of Document, DHEW Publication No. (NIH) 79-720, p. 35.
- ^ "The History of Cancer". American Cancer Society. September 2009. http://www.cancer.org/docroot/CRI/content/CRI_2_6x_the_history_of_cancer_72.asp.
- ^ Marilyn Yalom "A history of the breast" 1997. New York: Alfred A. Knopf. ISBN 0-679-43459-3
- ^ Grange JM, Stanford JL, Stanford CA (2002). "Campbell De Morgan's 'Observations on cancer', and their relevance today". Journal of the Royal Society of Medicine 95 (6): 296–9. doi:10.1258/jrsm.95.6.296. PMC 1279913. PMID 12042378. http://jrsm.rsmjournals.com/cgi/reprint/95/6/296.pdf.
- ^ Boveri, Theodor (2008). "Concerning The Origin of Malignant Tumours". Journal of Cell Science 121 (Supplement 1): 1–84. doi:10.1242/jcs.025742. PMID 18089652. http://jcs.biologists.org/cgi/content/full/121/Supplement_1/1.
- ^ Ehrenreich, Barbara (November 2001). "Welcome to Cancerland". Harper's Magazine. ISSN 0017-789X. http://www.barbaraehrenreich.com/cancerland.htm.
- ^ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ^ "Skin cancers". World Health Organization. http://www.who.int/uv/faq/skincancer/en/index1.html. Retrieved 19 January 2011.
- ^ McCulley, Michelle; Greenwell, Pamela (2007). Molecular therapeutics: 21st-century medicine. London: J. Wiley. p. 207. ISBN 0-470-01916-6.
- ^ Gwyn, Richard (1999). "10". In Cameron, Lynne; Low, Graham. Researching and applying metaphor. Cambridge, UK: Cambridge University Press. ISBN 0-521-64964-1.
- ^ Sulik, Gayle (2010). Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. New York: Oxford University Press. pp. 78–89. ISBN 0199740453. OCLC 535493589.
- ^ a b c d Ehrenreich, Barbara (2009). Bright-sided: How the Relentless Promotion of Positive Thinking Has Undermined America. New York: Metropolitan Books. pp. 15–44. ISBN 0-8050-8749-4.
- ^ Sharon Begley (2008-09-16). "Rethinking the War on Cancer". Newsweek. http://www.newsweek.com/id/157548/page/2. Retrieved 2008-09-08.
- ^ Kolata, Gina (April 23, 2009). "Advances Elusive in the Drive to Cure Cancer". The New York Times. http://www.nytimes.com/2009/04/24/health/policy/24cancer.html. Retrieved 2009-05-05.
- ^ a b c d e f g h i j Connie Henke Yarbro, Debra Wujcik, Barbara Holmes Gobel, ed (2011). Cancer nursing: principles and practice (7 ed.). Jones & Bartlett Publishers. pp. 901–905. ISBN 9781449618292.
Further reading
- Kleinsmith, Lewis J. (2006). Principles of cancer biology. Pearson Benjamin Cummings. ISBN 978-0-8053-4003-7. http://books.google.com/books?id=LKVrAAAAMAAJ. Retrieved 6 September 2011.
- Mukherjee, Siddhartha (16 November 2010). The Emperor of All Maladies: A Biography of Cancer. Simon and Schuster. ISBN 978-1-4391-0795-9. http://books.google.com/books?id=5rF_31RVTnMC. Retrieved 6 September 2011.
- Parkin D, Bray F, Ferlay J, Pisani P (2005). "Global cancer statistics, 2002" (PDF). CA Cancer J Clin 55 (2): 74–108. doi:10.3322/canjclin.55.2.74. PMID 15761078. http://caonline.amcancersoc.org/cgi/reprint/55/2/74.
- Pazdur, Richard; et al. (May 2009). Cancer Management: A Multidisciplinary Approach. Cmp United Business Media. ISBN 978-1-891483-62-2. http://books.google.com/books?id=wbLnPAAACAAJ. Retrieved 6 September 2011. (online at cancernetwork.com)
- Tannock, Ian (2005). The basic science of oncology. McGraw-Hill Professional. ISBN 978-0-07-138774-3. http://books.google.com/books?id=Bb4F4pj2BdYC. Retrieved 6 September 2011.
- Weinberg, Robert A. (September 1996). "How Cancer Arises: An explosion of research is uncovering the long-hidden molecular underpinnings of cancer—and suggesting new therapies" (PDF). Scientific American: 62–70. http://cns.uni.edu/~spradlin/genetics/Weinberg.pdf. "Introductory explanation of cancer biology in layman's language"
- Manfred Schwab (2008). Encyclopedia of Cancer (4 Volume Set). Berlin: Springer. ISBN 3-540-36847-7.
External links
- Cancer at the Open Directory Project
Pathology: Tumor, Neoplasm, Cancer, and Oncology (C00–D48, 140–239) Conditions Malignant progressionTopographyHead/Neck (Oral, Nasopharyngeal) · Digestive system · Respiratory system · Bone · Skin · Blood · Urogenital · Nervous system · Endocrine systemHistologyOtherPrecancerous condition · Paraneoplastic syndromeStaging/grading Carcinogenesis Misc. M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Carcinogen—Cancer causing materials and agents Main articles Cancer · Cancer cellsMajor suspected carcinogens IARC International Agency for Research on Cancer / IARC agent lists: Group 1 · Group 2A · Group 2B · Group 3 · Group 4 (Caprolactam)Categories:- Aging-associated diseases
- Causes of death
- Deaths from cancer
- Occupational safety and health
- Oncology
- Pathology
- Types of neoplasia
Wikimedia Foundation. 2010.