- Acupuncture
-
Acupuncture Intervention 
Needles being inserted into a patient's skin.ICD-10-PCS 8E0H30Z ICD-9: 99.91-99.92 MeSH D015670 OPS-301 code: 8-975.2 Alternative medical systems Acupuncture · Anthroposophic medicine · Ayurveda · Chiropractic · Herbalism · Homeopathy · Naturopathy · Qigong · Siddha medicine · Traditional medicine
(Chinese · Mongolian · Tibetan) · UnaniNCCAM classifications Whole medical systems · Mind-body interventions · Biologically based therapies · Manipulative therapy · Energy therapies See also Alternative medicine · Glossary · People Energy medicine - edit NCCAM classifications - Alternative Medical Systems
- Mind-Body Intervention
- Biologically Based Therapy
- Manipulative Methods
- Energy Therapy
See also Acupuncture is a type of alternative medicine that treats patients by insertion and manipulation of solid, generally thin needles in the body.
Through its origins, acupuncture has been embedded in the concepts of Traditional Chinese medicine (TCM). Its general theory is based on the premise that bodily functions are regulated by the flow of an energy-like entity called qi. Acupuncture aims to correct imbalances in the flow of qi by stimulation of anatomical locations on or under the skin called acupuncture points, most of which are connected by channels known as meridians. Scientific research has failed to validate the existence of any of the TCM concepts[1][2][3][4][5] and some contemporary practitioners needle the body without using a theoretical framework, instead selecting points based on their tenderness to pressure.[6]
The earliest written record of acupuncture is found in the Huangdi Neijing (黄帝内经; translated as The Yellow Emperor's Inner Canon), dated approximately 200 BCE.[7] The practice of acupuncture expanded out of China into the areas now part of Japan, Korea and Taiwan, diverging from the narrower theory and practice of mainland TCM in the process.[8] A large number of contemporary practitioners outside of China, particularly Europe, follow these non-TCM practices.[9] The most notable difference is that these other approaches often are primarily acupuncture, and do not incorporate Chinese herbal medicine.[citation needed]
Acupuncture proponents have claimed that it promotes general health, relieves pain, treats infertility, treats and prevents disease.[10] Meanwhile, evidence for its effectiveness for anything but the relief of some types of pain and nausea has not been established.[11][12][13][14][1][15] Systemic reviews have found conflicting results regarding the prevention of postoperative nausea and vomiting[16][17] though a 2009 Cochrane review concluded stimulation of the P6 acupuncture point was as effective as antiemetic medications.[17] Acupuncture also appears to have a small effect in the short-term management of some types of pain[13][18][19] though a 2011 review of review articles concluded that, except for neck pain, acupuncture was of doubtful efficacy.[15] It has been suggested that the positive results reported for acupuncture can be explained by placebo effects and publication bias[1][18][20][21][22] and researchers have pointed out the difficulty in designing an adequate scientific control for any placebo effect acupuncture might have due to its invasiveness.[2][11][23][24][25] The development and inclusion of retracting needles as a form of placebo control has resulted in a much larger number of studies concluding acupuncture's effects are due to placebo.[13]
There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles[2][26][27][28] but does carry small but serious risks and adverse effects including death.[15] Accompanied by calls for more research, the use of acupuncture for certain conditions has been tentatively endorsed by the United States National Institutes of Health[2] and National Center for Complementary and Alternative Medicine,[26] the National Health Service of the United Kingdom,[29] and the World Health Organization,[30] though most of these endorsements have been criticized[31][32][33] and it has been questioned whether research on acupuncture is a good use of limited research funding.[34][2][26][27][28][35]
Contents
History
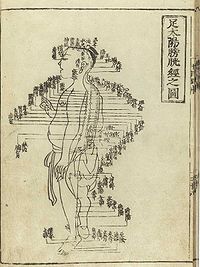
 Acupuncture chart from the Ming Dynasty (c. 1368–1644)
Acupuncture chart from the Ming Dynasty (c. 1368–1644)
Antiquity
In China, the earliest examples of metal needles were found in a tomb dated to c. 113 BCE, are believed to be used for medicinal purposes though not necessarily acupuncture. The earliest example of the unseen meridians used for diagnosis and treatment are dated to the second century BCE but these records do not mention needling, while the earliest reference to therapeutic needling occurs in the historical Shiji text (史記, English: Records of the Grand Historian) but does not mention the meridians and may be a reference to lancing rather than acupuncture.[36] The 2nd century BCE medical text Huangdi Neijing (黃帝內經, English: Yellow Emperor's Inner Canon) combines acupuncture with moxibustion[7] and may refer to the use of needles to drain water from joints or lance abscesses (though the Huangdi Neijing has been revised several times since its original publication in, and the oldest version currently available dates to the 11 century of the Common Era).[36]
Acupuncture's origins in China are uncertain. One explanation is that some soldiers wounded in battle by arrows were believed to have been cured of chronic afflictions that were otherwise untreated,[37] and there are variations on this idea.[38] Sharpened stones known as Bian shi have been found in China, suggesting the practice may date to the Neolithic[39] or possibly even earlier in the Stone Age.[40] Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) which suggest that acupuncture was practiced along with moxibustion.[41] It has also been suggested that acupuncture has its origins in bloodletting[42] or demonology.[7]
Despite improvements in metallurgy over centuries, it was not until the 2nd century BCE during the Han Dynasty that stone and bone needles were replaced with metal.[39] The earliest records of acupuncture is in the Shiji (史記, in English, Records of the Grand Historian) with references in later medical texts that are equivocal, but could be interpreted as discussing acupuncture. The earliest Chinese medical text to describe acupuncture is the Huangdi Neijing, the legendary Yellow Emperor's Classic of Internal Medicine (History of Acupuncture) which was compiled around 305–204 BCE.[7]
The Huangdi Neijing does not distinguish between acupuncture and moxibustion and gives the same indication for both treatments. The Mawangdui texts, which also date from the 2nd century BCE (though antedating both the Shiji and Huangdi Neijing), mention the use of pointed stones to open abscesses, and moxibustion but not acupuncture. However, by the 2nd century BCE, acupuncture replaced moxibustion as the primary treatment of systemic conditions.[7]
In Europe, examinations of the 5,000-year-old mummified body of Ötzi the Iceman have identified 15 groups of tattoos on his body, some of which are located on what are now seen as contemporary acupuncture points. This has been cited as evidence that practices similar to acupuncture may have been practiced elsewhere in Eurasia during the early Bronze Age.[43]
Middle history
 Acupuncture chart from Hua Shou (fl. 1340s, Ming Dynasty). This image from Shi si jing fa hui (Expression of the Fourteen Meridians). (Tokyo: Suharaya Heisuke kanko, Kyoho gan 1716).
Acupuncture chart from Hua Shou (fl. 1340s, Ming Dynasty). This image from Shi si jing fa hui (Expression of the Fourteen Meridians). (Tokyo: Suharaya Heisuke kanko, Kyoho gan 1716).
Acupuncture spread from China to Korea, Japan and Vietnam and elsewhere in East Asia.
Around ninety works on acupuncture were written in China between the Han Dynasty and the Song Dynasty, and the Emperor Renzong of Song, in 1023, ordered the production of a bronze statuette depicting the meridians and acupuncture points then in use. However, after the end of the Song Dynasty, acupuncture lost status, and started to be seen as a technical profession, in comparison to the more scholarly profession of herbalism. It became rarer in the following centuries, and was associated with less prestigious practices like alchemy, shamanism, midwifery and moxibustion.[44]
Portuguese missionaries in the 16th century were among the first to bring reports of acupuncture to the West.[45] Jacob de Bondt, a Dutch surgeon traveling in Asia, described the practice in both Japan and Java. However, in China itself the practice was increasingly associated with the lower-classes and illiterate practitioners.[46]
In 1674, Hermann Buschoff, a Dutch priest in Batavia, published the first book on moxibustion (from Japanese mogusa) for the cure of arthritis. The first elaborate Western treatise on acupuncture was published in 1683 by Willem ten Rhijne, a Dutch physician who had worked at the Dutch trading post Dejima in Nagasaki for two years.[47] In 1757 the physician Xu Daqun described the further decline of acupuncture, saying it was a lost art, with few experts to instruct; its decline was attributed in part to the popularity of prescriptions and medications, as well as its association with the lower classes.[48]
In 1822, an edict from the Chinese Emperor banned the practice and teaching of acupuncture within the Imperial Academy of Medicine outright, as unfit for practice by gentlemen-scholars. At this point, acupuncture was still cited in Europe with both skepticism and praise, with little study and only a small amount of experimentation.[49]
Modern era
In the early years after the Chinese Civil War, Chinese Communist Party leaders ridiculed traditional Chinese medicine, including acupuncture, as superstitious, irrational and backward, claiming that it conflicted with the Party's dedication to science as the way of progress. Communist Party Chairman Mao Zedong later reversed this position, saying that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level."[50] Under Mao's leadership, in response to the lack of modern medical practitioners, acupuncture was revived and its theory rewritten to adhere to the political, economic and logistic necessities of providing for the medical needs of China's population. Despite Mao proclaiming the practice of Chinese medicine to be "scientific", the practice was based more on the materialist assumptions of Marxism in opposition to superstition rather than the Western practice of empirical investigation of nature. Later the 1950s TCM's theory was again rewritten at Mao's insistence as a political response to the lack of unity between scientific and traditional Chinese medicine, and to correct the supposed "bourgeois thought of Western doctors of medicine" (p. 109).[51]
Acupuncture gained attention in the United States when President Richard Nixon visited China in 1972. During one part of the visit, the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia. Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients.[52]
The greatest exposure in the West came when New York Times reporter James Reston, who accompanied Nixon during the visit, received acupuncture in China for post-operative pain after undergoing an emergency appendectomy under standard anesthesia. Reston experienced pain relief from the acupuncture and wrote it in The New York Times.[53] In 1973 the American Internal Revenue Service allowed acupuncture to be deducted as a medical expense.[54]
In 2006, a BBC documentary Alternative Medicine filmed a patient undergoing open heart surgery allegedly under acupuncture-induced anesthesia. It was later revealed that the patient had been given a cocktail of weak anesthetics that in combination could have a much more powerful effect. The program was also criticized for its fanciful interpretation of the results of a brain scanning experiment.[1][55][56]
The use of acupuncture as anesthesia for surgery has fallen out of favor with scientifically trained surgeons in China. A delegation of the Committee for Skeptical Inquiry reported in 1995: We were not shown acupuncture anesthesia for surgery, this apparently having fallen out of favor with scientifically trained surgeons. Dr. Han, for instance, had been emphatic that he and his colleagues see acupuncture only as an analgesic (pain reducer), not an anesthetic (an agent that blocks all conscious sensations).[52]
Theory
The general theory of acupuncture is based on the premise that bodily functions are regulated by an energy called qi which flows through the body; disruptions of this flow are believed to be responsible for disease.[2] Acupuncture describes a family of procedures aiming to correct imbalances in the flow of qi by stimulation of anatomical locations on or under the skin (usually called acupuncture points or acupoints), by a variety of techniques.[2] The most common mechanism of stimulation of acupuncture points employs penetration of the skin by thin metal needles, which are manipulated manually or by electrical stimulation.[2]
Qi, meridians and acupuncture points
Main articles: Traditional Chinese medicine#TCM model of the body, Meridian (Chinese medicine), and Acupuncture pointOld Chinese medical chart on acupuncture meridians
Traditional Chinese medicine distinguishes not only one but several different kinds of qi (氣).[57] In a general sense, qi is something that is defined by five "cardinal functions":[57][58]
- Actuation (推動, tuīdòng) - of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians.
- Warming (溫煦, pinyin: wēnxù) - the body, especially the limbs.
- Defense (防御, pinyin: fángyù) - against Exogenous Pathogenic Factors
- Containment (固攝, pinyin: gùshè) - of body fluids, i.e. keeping blood, sweat, urine, semen etc. from leakage or excessive emission.
- Transformation (氣化, pinyin: qìhuà) - of food, drink, and breath into qi, xue (blood), and jinye (“fluids”), and/or transformation of all of the latter into each other.
To fulfill its functions, qi has to steadily flow from the inside of the body (where the zang-fu organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints. It is assisted in its flow by "channels" referred to as meridians (经络, pinyin: jīng-luò). TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài) respectively.[59] There's also a number of less customary channels branching off from the "regular" meridians.[60] No contemporary research has supported the existence of qi or meridians.[1][4][5] The meridians are believed to connect to the bodily organs, of which those considered hollow organs (such as the stomach and intestines) were also considered yang while those considered solid (such as the liver and lungs) were considered yin. They were also symbolically linked to the rivers found in ancient China, such as the Yangtze, Wei and Yellow Rivers.[61]
Acupuncture points are mainly (but not always) found at specified locations along the meridians. There also is a number of acupuncture points with specified locations outside of the meridians; these are called "extraordinary" points and often credited with special therapeutic properties. A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes.[62] The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in Han times, the number of bones thought to be in the body). The Huangdi Neijing mentioned only 160 and a further 135 could be deduced giving a total of 295. The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions. In addition, it is considered likely that some points used historically have since ceased being used.[63]
TCM concept of disease
Main article: Traditional Chinese medicine#Concept of diseaseIn TCM, disease is generally perceived as a disharmony (or imbalance) in the functions or interactions of yin, yang, qi, xuĕ, zàng-fǔ, meridians etc. and/or of the interaction between the human body and the environment.[64] Therapy is based on which "pattern of disharmony" can be identified.[65][66] In the case of the meridians, typical disease patterns are invasions with wind, cold and damp Excesses.[67]
In order to determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing or the sound of the voice.[68][69]
TCM and its concept of disease do not strongly differentiate between cause and effect.[70] In theory, however, endogenous, exogenous and miscellaneous causes of disease are recognized.[71]
Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient in order to make a diagnosis according to the tradition which he or she utilizes. In TCM, there are four diagnostic methods: inspection, auscultation and olfaction, inquiring, and palpation.[72]
- Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
- Auscultation and olfaction refer, respectively, to listening for particular sounds (such as wheezing) and attending to body odor.
- Inquiring focuses on the "seven inquiries", which are: chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea.
- Palpation includes feeling the body for tender A-shi points, and palpation of the left and right radial pulses at two levels of pressure (superficial and deep) and three positions Cun, Guan, Chi (immediately proximal to the wrist crease, and one and two fingers' breadth proximally, usually palpated with the index, middle and ring fingers).
Tongue and pulse
Examination of the tongue and the pulse are among the principal diagnostic methods in traditional Chinese medicine. The surface of the tongue is believed to contain a map of the entire body, and is used to determine acupuncture points to manipulate. For example, teeth marks on one part of the tongue might indicate a problem with the heart, while teeth marks on another part of the tongue might indicate a problem with the liver.[68] TCM diagnosis also involves measuring for three superficial and three deep pulses at different locations on the radial artery of each arm, for a total of twelve pulses that are thought to correspond to twelve internal organs. The pulse is examined for several characteristics including rhythm, strength and volume, and described with terms like "floating, slippery, bolstering-like, feeble, thready and quick", which are used to ascribe a specific imbalance in the body. Learning TCM pulse diagnosis can take several years.[73]
Clinical practice
In a modern acupuncture session, an initial consultation is followed by taking the pulse on both arms, and an inspection of the tongue. Classically, in clinical practice, acupuncture is highly individualized and based on philosophy and intuition, and not on controlled scientific research.[74] In the United States, acupuncture typically lasts from 10 to 60 minutes, with diagnosis and treatment for a single session ranging from $25 to $80 in 2011.[75] Sometimes needles are left in the ear for up to 3 days.[75]
Clinical practice varies depending on the country.[13][76] A comparison of the average number of patients treated per hour found significant differences between China (10) and the United States (1.2).[77] Aucpuncture is used to treat various type of pain, neurological problems and stroke rehabilitation.[77][78][79] Studies conducted in China and Brazil found that the majority of patients were female,[79] though in one study the majority of Chinese patients using acupuncture for stroke rehabilitation were male.[77]
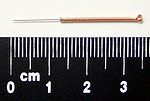
Needles
Acupuncture needles are typically made of stainless steel wire. They are usually disposable, but reusable needles are sometimes used as well, though they must be sterilized between uses.[80] Needles vary in length between 13 to 130 millimetres (0.51 to 5.1 in), with shorter needles used near the face and eyes, and longer needles in more fleshy areas; needle diameters vary from 0.16 mm (0.006 in) to 0.46 mm (0.018 in),[81] with thicker needles used on more robust patients. Thinner needles may be flexible and require tubes for insertion. The tip of the needle should not be made too sharp to prevent breakage, although blunt needles cause more pain.[82]
Apart from the usual filiform needle, there also other needle types which can be utilized, such as three-edged needles and the Nine Ancient Needles.[81] Japanese acupuncturists use extremely thin needles that are used superficially, sometimes without penetrating the skin, and surrounded by a guide tube (a technique adopted in China and the West). Korean acupuncture uses copper needles and has a greater focus on the hand.[76]
Needling technique
Insertion
Since most pain is felt in the superficial layers of the skin, a quick insertion of the needle is recommended. If skilled enough, a practitioner purportedly can insert the needles without causing any pain.[83]
Both peer-reviewed medical journals, and acupuncture journals reviewed by acupuncturists, have published on the painfulness of acupuncture treatments, in some cases within the context of reporting studies testing acupuncture’s effectiveness.[84][85][86][87] A peer-reviewed medical journal on pain published an article stating that "acupuncture is a painful and unpleasant treatment".[87] There are other cases in which patients have found the insertion of needles in acupuncture too painful to endure.[85] An acupuncture journal, peer-reviewed by acupuncturists, published an article describing insertion of needles in TCM acupuncture and random needling acupuncture as “painful stimulation”.[88] In a peer-reviewed medical journal, one medical scientist published that Japanese acupuncture is “far less painful” than Chinese acupuncture, and that Japanese acupuncture needles are smaller than Chinese acupuncture needles.[84]
De-qi sensation
De-qi (Chinese: 得气; pinyin: dé qì; lit. "obtaining of qi", usually translated as "arrival of qi") refers to a sensation of numbness, distension, or electrical tingling at the needling site which might radiate along the corresponding meridian. If it can not be generated, inaccurate location of the acupoint, improper depth of needle insertion, inadequate manipulation, or a very weak constitution of the patient have to be considered, all of which decrease the likelihood of successful treatment. If de-qi sensation doesn't immediately occur upon needle insertion, various manipulation techniques can be applied to promote it (such as "plucking", "shaking" or "trembling"). Once it is achieved, further techniques might be utilized which aim to influence the de-qi; for example, by certain manipulation the de-qi sensation allegedly can be conducted from the needling site towards more distant sites of the body. Other techniques aim at "tonifying" (Chinese: 补; pinyin: bǔ) or "sedating" (Chinese: 泄; pinyin: xiè) qi.[81] The former techniques are used in vacuity patterns, the latter in repletion patterns.[89]
De qi is more important in Chinese acupuncture, while Western and Japanese patients may not consider it a necessary part of the treatment.[76]
Related practices
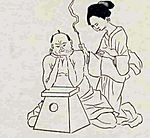
- Moxibustion – Acupuncture is often accompanied by moxibustion, the burning of cone-shaped preparations of Artemisia vulgaris (mugwort) on or near the skin, often but not always near or on an acupuncture point. Traditionally acupuncture was used to treat acute conditions while moxibustion was used for chronic diseases. Moxibustion could be direct (the cone was placed directly on the skin and allowed to burn the skin producing a blister and eventually a scar), or indirect (either a cone of mugwort was placed on a slice of garlic, ginger or other vegetable, or a cylinder of mugwort was held above the skin, close enough to either warm or burn it).[90]
- Fire cupping
- Tuina (also known as acupressure) is a TCM method of attempting to stimulate the flow of qi by various bare handed techniques.
- Electroacupuncture is a form of acupuncture in which acupuncture needles are attached to a device that generates continuous electric pulses. Another term is percutaneous electrical nerve stimulation.
- Sonopuncture or acutonics is a stimulation of the body similar to acupuncture, but using sound instead of needles.[91] This may be done using purpose-built transducers to direct a narrow ultrasound beam to a depth of 6–8 centimetres at acupuncture meridian points on the body.[92] Alternatively, tuning forks or other sound emitting devices are used.[93]
- Acupuncture point injection is the injection of various substances (such as drugs, vitamins or herbal extracts into acupuncture point.[94]
- Ear acupuncture is a form of acupuncture developed in France which is based on the assumption of reflexological representation of the entire body in the outer ear.[34]
- Scalp acupuncture is likewise based on reflexological considerations regarding the scalp area; it has been developed in Japan.[34]
- Hand acupuncture similarly centers around assumed reflex zones of the hand; it has been developed in Korea.[34]
- Medical acupuncture tries to integrate reflexological concepts, the trigger point model, and anatomical insights (such as dermatome distribution) into acupuncture practice, and emphasizes a more formulaic approach to acupuncture point location.[34]
- Cosmetic acupuncture is the use of acupuncture in an attempt to reduce wrinkles on the face.[95]
Effectiveness for specific conditions
Professor of Complementary and Alternative Medicine Edzard Ernst and his colleagues have produced regular systematic reviews of the acupuncture literature. In 2007, they concluded that "the emerging clinical evidence seems to imply that acupuncture is effective for some but not all conditions."[11] Several review articles discussing the effectiveness of acupuncture have concluded that its effects may be due to placebo.[13][18][19] Evidence for the treatment of psychological conditions other than pain is equivocal.[11] Acupuncture's greatest effectiveness appears to be in symptomatic control of pain and nausea.
Pain
A 2009 review of the highest quality clinical trials of acupuncture in the treatment of pain, published in the British Medical Journal, reported a "small analgesic effect of acupuncture was found, which seems to lack clinical relevance and cannot be clearly distinguished from bias. Whether needling at acupuncture points, or at any site, reduces pain independently of the psychological impact of the treatment ritual is unclear."[19] A 2011 review of fifty seven systematic reviews of the topic, published in the journal of the International Association for the Study of Pain found there is "little truly convincing evidence that acupuncture is effective in reducing pain."[15] A review of Cochrane Collaboration articles on pain concluded that "Their results suggest that acupuncture is effective for some but not all types of pain" and singled out migraines, neck disorders, tension headaches, and peripheral joint osteoarthritis as having evidence supporting acupuncture's use, while results were inconclusive for shoulder pain, lateral elbow pain, and low back pain and negative for rheumatoid arthritis.[96] Medical acupuncturist Steven E. Braverman, who separates the "needling" of acupuncture from its theoretical basis within traditional Chinese medicine, stated in 2004 that he believed needling has been successful in treating some pain and recommended acupuncture be considered a complementary therapy for various conditions. Braverman and other medical acupuncturists also stated that definitive conclusions based on research findings were rare because the state of acupuncture research is poor, but that it is improving.[34]
For acute low back pain, there is insufficient evidence to recommend for or against either acupuncture or dry needling, though for chronic low back pain, acupuncture is more effective than other CAM treatments, but no more effective than conventional and alternative treatments for short-term pain relief and improving function. However, when combined with other conventional therapies, the combination is slightly better than conventional therapy alone.[18][97] A review for the American Pain Society/American College of Physicians found fair evidence that acupuncture is effective for chronic low back pain.[98] Conducting research on low back pain is unusually problematic since most patients have experienced "conventional care" – which is itself relatively ineffective[citation needed] – and have low expectations for it. As such, conventional care groups may not be an adequate scientific control and may even lead to nocebo effects that can further inflate of the apparent effectiveness of acupuncture.[99]
There is moderate evidence that for neck pain, acupuncture is more likely to be effective than other CAM treatments and offers short-term improvement compared to those on a waiting list.[100] This is tentatively supported by a recent review.[15]
There is evidence to support the use of acupuncture to treat headaches that are idiopathic, though the evidence is not conclusive and more studies need to be conducted.[101] Several trials have indicated that migraine patients benefit from acupuncture, although the correct placement of needles seems to be less relevant than is usually thought by acupuncturists. Overall in these trials acupuncture was associated with slightly better outcomes and fewer adverse effects than prophylactic drug treatment.[102]
There is conflicting evidence that acupuncture may be useful for osteoarthritis of the knee, with both positive[103][104] and negative[105] results. The Osteoarthritis Research Society International released a set of consensus recommendations in 2008 that concluded acupuncture may be useful for treating the symptoms of osteoarthritis of the knee.[106] Results for osteoarthritis in other joints suggest insignificant effects in short-term pain relief, which may be due to placebo or expectation effects.[107]
Nausea and vomiting
Stimulation of a particular acupuncture point (P6, located on the underside of the forearm, several finger-widths from the wrist) is traditionally thought to relieve nausea. A 2004 Cochrane Review initially concluded that acupuncture appeared to be more effective than antiemetic drugs in treating postoperative nausea and vomiting,[108] but the authors subsequently retracted this conclusion due to a publication bias in Asian countries that had skewed their results.[20] An updated Cochrane Review published in 2009 concluded that both penetrative and non-penetrative stimulation of the P6 acupuncture point was approximately equal to, but not better than, preventive antiemetic drugs for postoperative nausea and vomiting though only 10% of the studies had adequate information on patient blinding regarding receiving standard or nonstandard acupuncture.[17] A 2011 Cochrane Review on the treatment of vomiting after the start of chemotherapy concluded that acupuncture point stimulation with needles and electroacupuncture reduced the number times subjects vomited on the day of treatment, but were no help regarding immediate or delayed nausea. Acupressure was found to reduce the short-term severity of nausea, but was no help over the long term and did not influence vomiting. All of the experiments reviewed also used medication to control vomiting, though trials involving electroacupuncture did not use the newest drugs available.[109]
A 2008 review examined randomized controlled trials on the effects of the P6 point, as well as points thought to rely on the same meridian, at preventing PONV within the first 24 hours of surgery. Three of the ten studies found statistically significant evidence that acupuncture could prevent PONV though comparison of the studies is difficult due to the use of varied methodologies (different patient groups, different ways of stimulating the P6 point such as a needle versus finger pressure versus a special bracelet, timing and length of application of pressure, the use of one versus both arms, whether a general anaesthetic was used, and the mixture of men and women in the studies). The reviewer ultimately concluded that "due to the lack of robust studies, [this review] found that neither acupressure nor acupuncture was effective in preventing or managing PONV in adults" and suggested further research to clarify issues such as the length and type of stimulation applied, training of those applying stimulation and gathering data, risk factors for PONV, inclusion of proper placebos, and the analysis of specific population. The author also suggested disagreement with previous systemic reviews were due to their inclusion of older studies with poorer methodologies, while the more recent, better quality studies included in the review offered more negative results.[16]
Fertility and childbirth
Proponents believe acupuncture can assist with fertility, pregnancy and childbirth, attributing various conditions of health and difficulty with the flow of qi through various meridians.[110]
A 2008 Cochrane review of randomized controlled trials of in vitro fertilisation and acupuncture suggests that acupuncture performed on the day the embryo is transferred to the uterus may increase the live birth rate, although this effect could be due to the placebo effect and the small number of women included in acceptable trials. There was no evidence of benefit when the egg was initially removed and the review did not recommend the routine use of acupuncture during the luteal phase until better trials were available.[111] A different review article published in 2010 found that there was no evidence acupuncture improved pregnancy rates irrespective of when it was performed and recommended against its use during in vitro fertilization either during egg retrieval or implantation.[112][113]
Lack of effectiveness for other conditions
The Danish Knowledge and Research Center for Alternative Medicines has a fully updated list of all the Cochrane Collaboration regarding acupuncture [114] and the overall conclusion is:
...the majority of the Cochrane reviews about acupuncture, acupressure, electroacupuncture and moxibustion [concluded] there exists no solid evidence to determine the effectiveness of the treatments. The reviews point out that many of the studies suffer from methodological defects and shortcomings. Furthermore, the number of trial subjects has been limited. Thus most of the overall conclusions are uncertain.
For the following conditions, the Cochrane Collaboration or other review articles have concluded there is insufficient evidence to determine whether acupuncture is beneficial, often because of the paucity and poor quality of the research, and that further research is needed:
- Chronic asthma[115]
- Bell's palsy[116]
- Cocaine dependence[117]
- depression[118]
- Drug detoxification[119][120][121]
- Primary dysmenorrhoea (incorporating TENS)[122]
- Epilepsy[123]
- Fibromyalgia[124]
- Glaucoma,[125]
- Insomnia[126]
- Irritable bowel syndrome[127]
- Induction of childbirth[128]
- Rheumatoid arthritis[129]
- Shoulder pain[130]
- Schizophrenia[131]
- Smoking cessation[132]
- Acute stroke[133] and stroke rehabilitation[134]
- Tennis elbow[135]
- Vascular dementia[136]
Scientific basis
Acupuncture has been the subject of active scientific research both in regard to its basis and therapeutic effectiveness since the late 20th century, but it remains controversial among medical researchers and clinicians.[11] Research on acupuncture points and meridians has not demonstrated their existence or properties.[137] Clinical assessment of acupuncture treatments, due to its invasive and easily detected nature, makes it difficult to use proper scientific controls for placebo effects.[2][11][23][24][25] Positive results from some studies on the efficacy of acupuncture may be as a result of poorly designed studies or publication bias.[20][21][22] Edzard Ernst and Simon Singh state that (as the quality of experimental tests of acupuncture have increased over the course of several decades through better blinding, the use of sham needling as a form of placebo control, etc.) the "more that researchers eliminate bias from their trials, the greater the tendency for results to indicate that acupuncture is little more than a placebo."[1] Also complicating reseach on acupuncture is the possibility of a strong publication bias from certain countries; a review of studies on acupuncture found that trials originating in China, Japan, Hong Kong and Taiwan were uniformly favourable to acupuncture, as were ten out of 11 studies conducted in Russia.[138]
Different types of comparison are made in the scientific literature and terminology can vary, therefore care is needed when assessing research. “Acupuncture” may refer only to insertion of needles in traditionally determined acupuncture points; in which case, it is contrasted with randomly inserting needles, which is called a sham treatment, placebo, needling or medical acupuncture if the points are determined by anatomy and not by TCM. In some sources "acupuncture" refers to random needling with needle insertion, and this is compared to pressing telescoping needles against the skin at the same points but not puncturing the skin, which is called a "sham treatment" or "placebo".[34][2][35]
The World Health Organization[30] and the United States' National Institutes of Health (NIH)[2] have stated that acupuncture can be effective in the treatment of neurological conditions and pain, though these statements have been criticized for bias and a reliance on studies that used poor methodology.[1][32] Reports from the USA's National Center for Complementary and Alternative Medicine (NCCAM), the American Medical Association (AMA) and various USA government reports have studied and commented on the efficacy of acupuncture. There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles, but not on its efficacy as a medical procedure.[2][26][27][28]
Many research studies conclude that "further research is needed", but opinion is divided as to whether this is a good place to spend limited research funds.[34][2][26][27][28][35]
Criticism
The National Council Against Health Fraud stated in 1990 that acupuncture’s “theory and practice are based on primitive and fanciful concepts of health and disease that bear no relationship to present scientific knowledge.”[139] In 1993 neurologist Arthur Taub called acupuncture “nonsense with needles.”[140] The website Quackwatch criticizes TCM as having unproven efficacy and an unsound scientific basis.[141] Physicist John P. Jackson,[142] Steven Salzberg, director of the Center for Bioinformatics and Computational Biology and professor at the University of Maryland,[143] Yale University professor of neurology, and founder and executive editor of the blog Science Based Medicine, Steven Novella,[144] and Wallace Sampson, clinical professor emeritus of medicine at Stanford University and editor-in-chief at the Scientific Review of Alternative Medicine, have all characterized acupuncture as pseudoscience[145] or pseudomedical.[146]
According to the 1997 NIH consensus statement on acupuncture:
Despite considerable efforts to understand the anatomy and physiology of the "acupuncture points", the definition and characterization of these points remains controversial. Even more elusive is the basis of some of the key traditional Eastern medical concepts such as the circulation of Qi, the meridian system, and the five phases theory, which are difficult to reconcile with contemporary biomedical information but continue to play an important role in the evaluation of patients and the formulation of treatment in acupuncture.[2]Qi, acupuncture points and meridians
In some early texts, 365 acupuncture points were identified, corresponding to the days of the year.[147] No research has established any consistent anatomical structure or function for either acupuncture points or meridians.[1][5] The nervous system has been evaluated for a relationship to acupuncture points, but no structures have been clearly linked to them. Controversial studies using nuclear imaging have suggested that tracers may be used to follow meridians and are not related to veins or lymphatic tissues, but the interpretation of these results is unclear. The electrical resistance of acupuncture points and meridians have also been studied, with conflicting results.[5]
The meridians are part of the controversy in the efforts to reconcile acupuncture with conventional medicine. The National Institutes of Health 1997 consensus development statement on acupuncture stated that acupuncture points, Qi, the meridian system and related theories play an important role in the use of acupuncture, but are difficult to relate to a contemporary understanding of the body.[2] Chinese medicine forbade dissection, and as a result the understanding of how the body functioned was based on a system that related to the world around the body rather than its internal structures. The 365 "divisions" of the body were based on the number of days in a year, and the 12 meridians proposed in the TCM system are thought to be based on the 12 major rivers that run through China.[3]
The ancient traditions of qi, yin, yang and meridians have no counterpart in modern studies of chemistry, biology, physics, or human physiology and to date scientists have been unable to find evidence that supports their existence.[1][5] Support for the existence of qi is often looked for in scientific fields such as bioelectricity[148] but this research is rarely verified and the connection with qi may be spurious.
Research on the electrical activity of acupuncture points lacks a standardized methodology and reporting protocols, and is generally of poor quality.[149]
Acupuncturist Felix Mann, who was the author of the first comprehensive English language acupuncture textbook Acupuncture: The Ancient Chinese Art of Healing, has stated that "The traditional acupuncture points are no more real than the black spots a drunkard sees in front of his eyes" and compared the meridians to the meridians of longitude used in geography – an imaginary human construct.[150] Mann attempted to join up his medical knowledge with that of Chinese theory. In spite of his protestations about the theory, he was fascinated by it and trained many people in the west with the parts of it he borrowed. He also wrote many books on this subject. His legacy is that there is now a college in London and a system of needling that is known as "Medical Acupuncture". Today this college trains doctors and western medical professionals only. Reviewers Leonid Kalichman and Simon Vulfsons have described the use of dry needling of myofascial trigger points as an effective and low risk treatment modality.[151] A systematic review of acupuncture for pain found that there was no difference between inserting needles into "true" acupuncture on traditional acupuncture points versus "placebo" points not associated with any TCM acupuncture points or meridians. The review concluded that "A small analgesic effect of acupuncture was found, which seems to lack clinical relevance and cannot be clearly distinguished from bias. Whether needling at acupuncture points, or at any site, reduces pain independently of the psychological impact of the treatment ritual is unclear."[19]
A history of medical science article published in the journal Biocommunications states that "the Chinese drew mystical numerical associations, called the Da shu, or “great numbers.” It was no coincidence to the ancient Chinese, for example, that our four limbs matched the number of seasons and directions, and that in the one record of a human dissection on the body of the rebel Wangsun Qing, the hired butchers of his captor, Wang Mang, reported finding five zang (liver, gall bladder, heart, spleen, kidneys) corresponding to the five planets; 12 vessels circulating blood and air corresponding to the 12 rivers flowing toward the Central Kingdom; and 365 parts of the body, one for each day of the year (Lingshu 13/311 ), and the Ling shu cited says “There are 365 days in the year, while humans have 365 joints (or acupoints)... There are 12 channel rivers across the land, while humans have 12 channel” – Ling Shu[3][152]
A report for CSICOP on pseudoscience in China written by Wallace Sampson and Barry Beyerstein said:
A few Chinese scientists we met maintained that although Qi is merely a metaphor, it is still a useful physiological abstraction (e.g., that the related concepts of yin and yang parallel modern scientific notions of endocrinologic [sic] and metabolic feedback mechanisms). They see this as a useful way to unite Eastern and Western medicine. Their more hard-nosed colleagues quietly dismissed Qi as only a philosophy, bearing no tangible relationship to modern physiology and medicine.[153]Possible mechanisms
Evidence supports that stimulation of one acupuncture point reduces post-operative nausea and vomiting, although insertion of needles at that point does not increase the reduction over nonpenetrating stimulation,[17] and pain,[18] but evidence for the treatment of other conditions is equivocal,[11] and several review articles discussing the effectiveness of acupuncture have concluded it is possible to explain through the placebo effect.[13][19] Despite consistently failing to find a difference between real and sham acupuncture, much of the literature on the topic has consistently failed to consider placebo effect as an explanation for apparent effectiveness.[99] Endorphin release, stimulation of the peripheral nervous system, and pain mediation through the effects of other neuropeptides are thought to be the most likely explanations for the effects of the insertion of needles.[2] Publication bias is a significant concern when evaluating the literature. Other claims of efficacy have not been tested. Reports from the US National Center for Complementary and Alternative Medicine (NCCAM), the American Medical Association (AMA) and various US government reports have studied and commented on the efficacy (or lack thereof) of acupuncture. There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles.[2][26][27][28] The neural mechanisms underlying minute pain relief from insertion of needles are unknown, but it has been suggested that it may involve recruitment of the body's own pain reduction system, and an increased release of endorphins, serotonin, norepinephrine, or gamma-Aminobutyric acid.[154]
Efficacy study design
See also: GERACOne of the major challenges in acupuncture research is in the design of an appropriate placebo control group.[23] In trials of new drugs, double blinding is the accepted standard, but since acupuncture is a procedure rather than a pill, it is difficult to design studies in which both the acupuncturist and patient are blinded as to the treatment being given. The same problem arises in double-blinding procedures used in biomedicine, including virtually all surgical procedures, dentistry, physical therapy, etc. As the Institute of Medicine states: "Controlled trials of surgical procedures have been done less frequently than studies of medications because it is much more difficult to standardize the process of surgery. Surgery depends to some degree on the skills and training of the surgeon and the specific environment and support team available to the surgeon. A surgical procedure in the hands of a highly skilled, experienced surgeon is different from the same procedure in the hands of an inexperienced and unskilled surgeon... For many CAM modalities, it is similarly difficult to separate the effectiveness of the treatment from the effectiveness of the person providing the treatment."[25]:126 Acupuncture itself is also a very strong placebo, and can provoke extremely high expectations from patients and test subjects; this is particularly problematic for health problems like chronic low back pain, where conventional treatment is often relatively ineffective and may have been unsuccessfully used in the past. In situations like these, it may be inappropriate to consider "conventional care" a proper control intervention for acupuncture since patient expectations for conventional care are quite low.[99]
Blinding of the practitioner in acupuncture remains challenging. One proposed solution to blinding patients has been the development of "sham acupuncture", i.e., needling performed superficially or at non-acupuncture sites. Controversy remains over whether, and under what conditions, sham acupuncture may function as a true placebo, particularly in studies on pain, in which insertion of needles anywhere near painful regions may elicit a beneficial response.[2][24] A review in 2007 noted several issues confounding sham acupuncture: "Weak physiologic activity of superficial or sham needle penetration is suggested by several lines of research, including RCTs showing larger effects of a superficial needle penetrating acupuncture than those of a nonpenetrating sham control, positron emission tomography research indicating that sham acupuncture can stimulate regions of the brain associated with natural opiate production, and animal studies showing that sham needle insertion can have nonspecific analgesic effects through a postulated mechanism of “diffuse noxious inhibitory control”. Indeed, superficial needle penetration is a common technique in many authentic traditional Japanese acupuncture styles."[105] When "placebo needles" (in which the needle retracts into a handle rather than penetrating the skin) were introduced to the study of acupuncture, the majority of studies conducted using these needles concluded the effects of acupuncture were due to placebo.[13]
An analysis of 13 studies of pain treatment with acupuncture, published in January 2009 in the journal BMJ, concluded there was little difference in the effect of real, sham and no acupuncture.[19]
Medical organizations
In 1997, the American Medical Association Council on Scientific Affairs stated:
Critics contend that acupuncturists, including many traditionally trained physicians, merely stick needles in patients as a way to offer another form of treatment for which they can be reimbursed, since many insurance companies will do so. Critical reviews of acupuncture summarized by Hafner and others conclude that no evidence exists that acupuncture affects the course of any disease...Much of the information currently known about these therapies makes it clear that many have not been shown to be efficacious. Well-designed, stringently controlled research should be done to evaluate the efficacy of alternative therapies.[155]Also in 1997, the United States National Institutes of Health (NIH) issued a consensus statement on acupuncture that concluded that despite research on acupuncture being difficult to conduct, there was sufficient evidence to encourage further study and expand its use.[2] The consensus statement and conference that produced it were criticized by Wallace Sampson, founder of the Scientific Review of Alternative Medicine, writing for an affiliated publication of Quackwatch who stated the meeting was chaired by a strong proponent of acupuncture and failed to include speakers who had obtained negative results on studies of acupuncture. Sampson also stated he believed the report showed evidence of pseudoscientific reasoning.[31] In 2006 the NIH's National Center for Complementary and Alternative Medicine stated that it continued to abide by the recommendations of the 1997 NIH consensus statement, even if research is still unable to explain its mechanism.[26]
In 2003 the World Health Organization's Department of Essential Drugs and Medicine Policy produced a report on acupuncture. The report was drafted, revised and updated by Zhu-Fan Xie, the Director for the Institute of Integrated Medicines of Beijing Medical University. It contained, based on research results available in early 1999, a list of diseases, symptoms or conditions for which it was believed acupuncture had been demonstrated as an effective treatment, as well as a second list of conditions that were possibly able to be treated with acupuncture. Noting the difficulties of conducting controlled research and the debate on how to best conduct research on acupuncture, the report described itself as "...intended to facilitate research on and the evaluation and application of acupuncture. It is hoped that it will provide a useful resource for researchers, health care providers, national health authorities and the general public."[30] The coordinator for the team that produced the report, Xiaorui Zhang, stated that the report was designed to facilitate research on acupuncture, not recommend treatment for specific diseases.[32] The report was controversial; critics assailed it as being problematic since, in spite of the disclaimer, supporters used it to claim that the WHO endorsed acupuncture and other alternative medicine practices that were either pseudoscientific or lacking sufficient evidence-basis. Medical scientists expressed concern that the evidence supporting acupuncture outlined in the report was weak, and Willem Betz of SKEPP (Studie Kring voor Kritische Evaluatie van Pseudowetenschap en het Paranormale, the Study Circle for the Critical Evaluation of Pseudoscience and the Paranormal) said that the report was evidence that the "WHO has been infiltrated by missionaries for alternative medicine".[32] The WHO 2005 report was also criticized in the 2008 book Trick or Treatment for, in addition to being produced by a panel that included no critics of acupuncture at all, containing two major errors – including too many results from low-quality clinical trials, and including a large number of trials originating in China where, probably due to publication bias, no negative trials have ever been produced. In contrast, studies originating in the West include a mixture of positive, negative and neutral results. Ernst and Singh, the authors of the book, described the report as "highly misleading", a "shoddy piece of work that was never rigorously scrutinized" and stated that the results of high-quality clinical trials do not support the use of acupuncture to treat anything but pain and nausea.[33] Ernst also described the statement in a 2006 peer reviewed article as "Perhaps the most obviously over-optimistic overview [of acupuncture]", noting that of the 35 conditions that the WHO stated acupuncture was effective for, 27 of the systematic reviews that the WHO report was based on found that acupuncture was not effective for treating the specified condition.[13]
The National Health Service of the United Kingdom states that there is "reasonably good evidence that acupuncture is an effective treatment" for nausea, vomiting, osteoarthritis of the knee and several types of pain but "because of disagreements over the way acupuncture trials should be carried out and over what their results mean, this evidence does not allow us to draw definite conclusions". The NHS states there is evidence against acupuncture being useful for rheumatoid arthritis, smoking cessation and weight loss, and inadequate evidence for most other conditions that acupuncture is used for.[29]
Safety
Because acupuncture needles penetrate the skin, many forms of acupuncture are invasive procedures, and therefore not without risk. Injuries are rare among patients treated by trained practitioners in some countries.[28][156] Sometimes, needles are required by law to be sterile, disposable and used only once; in some places, needles may be reused if they are first resterilized, e.g. in an autoclave. When needles are contaminated, risk of bacterial or other blood-borne infection increases, as with re-use of any type of needle.[157]
Adverse events
Estimates of adverse effects due to acupuncture range from 671[158] to 1,137 per 10,000 treatments. The majority of adverse effects reported are minor, mainly slight haemorrhage (2.9%), haematoma (2.2%), and dizziness (1%).[27] A 2010 systematic review found that acupuncture has been associated with a possible total of up to 86 deaths over the years surveyed, most commonly due to pneumothorax.[159] Some reported adverse effects include 50 cases of bacterial infections, and more than 80 cases of hepatitis B since 1970.[157][160] A 2011 review that included many case reports of injuries stated that "ninety-five cases of severe adverse effects including 5 fatalities" were evident in the literature reviewed. "Pneumothorax and infections were the most frequently reported adverse effects."[15]
Other injury
Other risks of injury include: nerve injury, resulting from the accidental puncture of any nerve, brain damage or stroke, which is possible with very deep needling at the base of the skull,[161] kidney damage from deep needling in the low back. Haemopericardium, or puncture of the protective membrane surrounding the heart, which may occur with needling over a sternal foramen.[162]
Omitting modern medical care
Receiving alternative medicine as a replacement for standard modern medical care could result in inadequate diagnosis or treatment of conditions for which modern medicine has a better treatment record.
As with other alternative medicines, unethical or naïve practitioners may also induce patients to exhaust financial resources by pursuing ineffective treatment.[163][164] Profession ethical codes set by accrediting organizations such as the National Certification Commission for Acupuncture and Oriental Medicine require practitioners to make "timely referrals to other health care professionals as may be appropriate."[165] In Canada, public health departments in the provinces of Ontario and British Columbia regulate acupuncture.[166][167]
Legal and political status
Main article: Regulation of acupunctureUnited States
Those who specialize in Acupuncture and Oriental Medicine are usually referred to as "licensed acupuncturists", or L.Ac.'s. The abbreviation "Dipl. Ac." stands for "Diplomate of Acupuncture" and signifies that the holder is board-certified by the NCCAOM.[168] Twenty-three states require certification, according to that body.[169]
A poll of American doctors in 2005 showed that 59% believe acupuncture was at least somewhat effective for treatment of pain.[170] In 1996, the United States Food and Drug Administration changed the status of acupuncture needles from Class III to Class II medical devices, meaning that needles are regarded as safe and effective when used appropriately by licensed practitioners.[171][172] As of 2004, nearly 50% of Americans who were enrolled in employer health insurance plans were covered for acupuncture treatments.[173][174]
Canada
In Ontario, the practice of acupuncture is now regulated by the Traditional Chinese Medicine Act, 2006, S.O. 2006, chapter 27.[175] The government is in the process of establishing a college[176] whose mandate will be to oversee the implementation of policies and regulations relating to the profession.
United Kingdom
Acupuncturists are not a regulated profession. The principal body for professional standards in traditional/lay acupuncture is the British Acupuncture Council,[177] The British Medical Acupuncture Society[178] is an inter-disciplinary professional body for regulated health professional using acupuncture as a modality and there is the Acupuncture Association of Chartered Physiotherapists.[179]
Australia
Traditional/lay acupuncture is not a regulated health profession; traditional/lay acupuncture or Chinese Medicine was not included in the National Health Regulation Law.[180] Acupuncture will not be recognized as a profession in Australia but as a modality, either within Chinese Medicine / traditional Asian healing systems or within the scope of practice of regulated health professions. The practice of acupuncture is governed by a range of state / territory laws relating to consumer protection and infection control. Victoria is the only state of Australia with an operational registration board.[181] Currently acupuncturists in New South Wales are bound by the guidelines in the Public Health (Skin Penetration) Regulation 2000,[182] which is enforced at local council level. Other states of Australia have their own skin penetration acts.
New Zealand
Traditional/lay acupuncture is not a regulated health profession. Osteopaths have a scope of practice for Western Medical Acupuncture and Related Needling Techniques.[183] The state-owned Accident Compensation Corporation reimburses for acupuncture treatment by registered health care practitioners and some traditional/lay acupuncturists that belong to voluntary professional associations.[184]
See also
- Chinese herbology
- Auriculotherapy
- Colorpuncture
- Pressure point
- Susuk
- German Acupuncture Trials
Bibliography
- Aung, SKH; Chen WPD (2007). Clinical introduction to medical acupuncture. Thieme Medical Publishers. ISBN 978-1-58890-221-4. http://books.google.ca/books?id=I6NclaeDWjgC&printsec=frontcover&source=gbs_atb#v=onepage&q&f=false.
- Barnes, LL (2005). Needles, herbs, gods, and ghosts: China, healing, and the West to 1848. Harvard University Press. ISBN 0674018729. http://books.google.com/?id=jU0JMNtGWnIC&printsec=frontcover&q=.
- Cheng, X (1987). Chinese Acupuncture and Moxibustion (1st ed.). Foreign Languages Press. ISBN 7-119-00378-X.
- Needham, J; Lu GD (2002). Celestial lancets: a history and rationale of acupuncture and moxa. Routledge. ISBN 0700714588. http://books.google.ca/books?id=0-0tdqBr58cC&printsec=frontcover&source=gbs_atb#v=onepage&q&f=false.</ref>
- Singh, S; Ernst E (2008). Trick or treatment: The undeniable facts about alternative medicine. W. W. Norton & Company. ISBN 0393066616.
- Stux, G; Pomeranz P (1988). Basics of Acupuncture. Berlin: Springer-Verlag. ISBN 354053072x. http://books.google.com/books?id=hsjd5nterXQC&printsec=frontcover&source=gbs_atb#v=onepage&q&f=false.
- Wiseman, N; Ellis A (1996). Fundamentals of Chinese medicine. Paradigm Publications. ISBN 978-0-912111-44-5. http://books.google.com/books?id=3SOAjUt53UgC&printsec=frontcover&source=gbs_atb#v=onepage&q&f=false.
References
- ^ a b c d e f g h i Goddard B (2008). "2. The Truth about Acupuncture". In Singh S, Ernst E. Trick or Treatment: The Undeniable Facts about Alternative Medicine. pp. 39–90. http://books.google.com/books?id=TnDHoXyi388C&pg=PA39#v=onepage&q&f=false. Retrieved 2011-06-15.
- ^ a b c d e f g h i j k l m n o p q r s NIH Consensus Development Program (November 3–5, 1997). "Acupuncture --Consensus Development Conference Statement". National Institutes of Health. http://consensus.nih.gov/1997/1997Acupuncture107html.htm. Retrieved 2007-07-17.
- ^ a b c Camillia Matuk (2006). "Seeing the Body: The Divergence of Ancient Chinese and Western Medical Illustration". Journal of Biocommunication 32 (1). http://www.sesp.northwestern.edu/docs/publications/6074956944509ac426aaa6.pdf.
- ^ a b Felix Mann, quoted in Bauer, M (2006). "The Final Days of Traditional Beliefs? – Part One". Chinese Medicine Times 1 (4): 31. http://www.chinesemedicinetimes.com/section.php?xSec=122.
- ^ a b c d e Ahn, Andrew C.; Colbert, Agatha P.; Anderson, Belinda J.; Martinsen, ØRjan G.; Hammerschlag, Richard; Cina, Steve; Wayne, Peter M.; Langevin, Helene M. (2008). "Electrical properties of acupuncture points and meridians: A systematic review". Bioelectromagnetics 29 (4): 245–56. doi:10.1002/bem.20403. PMID 18240287.
- ^ de las Peñas, César Fernández; Arendt-Nielsen, Lars; Gerwin, Robert D (2010). Tension-type and cervicogenic headache: pathophysiology, diagnosis, and management. Jones & Bartlett Learning. pp. 251-4. ISBN 9780763752835.
- ^ a b c d e Prioreschi, P (2004). A history of Medicine, Volume 2. Horatius Press. pp. 147–8. ISBN 1888456019.
- ^ Fruehauf H (2010). "Chinese Medicine In Crisis: Science, Politics, And The Making Of "TCM"". http://chineseclassics.org/j/images/tcmcrisis.pdf. Retrieved 2011-06-15.
- ^ Hicks, Angela; Hicks, John; Mole, Peter (2004). Five Element Constitutional Acupuncture (1st ed.). London: Churchill Livingstone. pp. ix. ISBN o443071705.
- ^ Novak, Patricia D.; Dorland, Norman W.; Dorland, William Alexander Newman (1995). Dorland's Pocket Medical Dictionary (25th ed.). Philadelphia: W.B. Saunders. ISBN 0-7216-5738-9. OCLC 33123537.
- ^ a b c d e f g Ernst, E.; Pittler, MH; Wider, B; Boddy, K (2007). "Acupuncture: its evidence-base is changing.". The American Journal of Chinese Medicine 35 (1): 21–5. doi:10.1142/S0192415X07004588. PMID 17265547.
- ^ Cherkin, D. C.; Sherman, K. J.; Avins, A. L.; Erro, J. H.; Ichikawa, L.; Barlow, W. E.; Delaney, K.; Hawkes, R. et al. (2009). "A Randomized Trial Comparing Acupuncture, Simulated Acupuncture, and Usual Care for Chronic Low Back Pain". Archives of Internal Medicine 169 (9): 858–866. doi:10.1001/archinternmed.2009.65. PMC 2832641. PMID 19433697. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2832641.
- ^ a b c d e f g h Ernst, E. (2006). "Acupuncture - a critical analysis". Journal of Internal Medicine 259 (2): 125–137. doi:10.1111/j.1365-2796.2005.01584.x. PMID 16420542.
- ^ Shapiro R (2008). Suckers: How alternative medicine makes fools of us all. Vintage Books. OCLC 267166615.
- ^ a b c d e f Ernst, E.; Lee, M. S.; Choi, T. Y. (2011). "Acupuncture: Does it alleviate pain and are there serious risks? A review of reviews" (pdf). PAIN 152 (4): 755–764. doi:10.1016/j.pain.2010.11.004. PMID 21440191. http://www.dieutridau.com/thongtin/detai/acupuncture-does-it.pdf.
- ^ a b Abraham, J. (2008). "Acupressure and acupuncture in preventing and managing postoperative nausea and vomiting in adults". Journal of perioperative practice 18 (12): 543–551. PMID 19192550.
- ^ a b c d Lee A, Fan, LTY (2009). Lee, Anna. ed. "Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting". Cochrane Database of Systematic Reviews (Online) (2): CD003281. doi:10.1002/14651858.CD003281.pub3. PMID 15266478. http://www.cochrane.org/reviews/en/ab003281.html.
- ^ a b c d e Furlan, Andrea D; Van Tulder, Maurits W; Cherkin, Dan; Tsukayama, Hiroshi; Lao, Lixing; Koes, Bart W; Berman, Brian M (2005). Furlan, Andrea D. ed (pdf). Acupuncture and dry-needling for low back pain. pp. CD001351. doi:10.1002/14651858.CD001351.pub2. PMID 15674876. http://www.thecochranelibrary.com/userfiles/ccoch/file/Acupuncture_ancient_traditions/CD001351.pdf.
- ^ a b c d e f Madsen, M. V.; Gotzsche, P. C; Hrobjartsson, A. (2009). "Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups". BMJ 338: a3115. doi:10.1136/bmj.a3115. PMC 2769056. PMID 19174438. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2769056.
- ^ a b c Lee A, Copas JB, Henmi M, Gin T, Chung RC (2006). "Publication bias affected the estimate of postoperative nausea in an acupoint stimulation systematic review". J Clin Epidemiol. 59 (9): 980–3. doi:10.1016/j.jclinepi.2006.02.003. PMID 16895822.
- ^ a b Tang, JL; Zhan, SY; Ernst, E (1999). "Review of randomised controlled trials of traditional Chinese medicine.". BMJ (Clinical research ed.) 319 (7203): 160–1. PMC 28166. PMID 10406751. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=28166.
- ^ a b Vickers, A; Goyal, N; Harland, R; Rees, R (1998). "Do Certain Countries Produce Only Positive Results? A Systematic Review of Controlled Trials". Controlled Clinical Trials 19 (2): 159–66. doi:10.1016/S0197-2456(97)00150-5. PMID 9551280.
- ^ a b c White, A.R.; Filshie, J.; Cummings, T.M.; International Acupuncture Research Forum (2001). "Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding". Complementary Therapies in Medicine 9 (4): 237–245. doi:10.1054/ctim.2001.0489. PMID 12184353.
- ^ a b c Johnson, M. I (2006). "The clinical effectiveness of acupuncture for pain relief – you can be certain of uncertainty". Acupuncture in Medicine 24 (2): 71–9. doi:10.1136/aim.24.2.71. PMID 16783282.
- ^ a b c Committee on the Use of Complementary and Alternative Medicine by the American Public (2005). Complementary and Alternative Medicine in the United States. National Academies Press. http://www.nap.edu/catalog.php?record_id=11182
- ^ a b c d e f g "Acupuncture". US National Center for Complementary and Alternative Medicine. 2006. http://nccam.nih.gov/health/acupuncture/. Retrieved 2006-03-02.
- ^ a b c d e f Ernst, G; Strzyz, H; Hagmeister, H (2003). "Incidence of adverse effects during acupuncture therapy—a multicentre survey". Complementary Therapies in Medicine 11 (2): 93–7. doi:10.1016/S0965-2299(03)00004-9. PMID 12801494.
- ^ a b c d e f Lao L, Hamilton GR, Fu J, Berman BM (2003). "Is acupuncture safe? A systematic review of case reports". Alternative therapies in health and medicine 9 (1): 72–83. PMID 12564354.
- ^ a b "Acupuncture: Evidence for its effectiveness". National Health Service. 2010-03-18. http://www.nhs.uk/Conditions/Acupuncture/Pages/Evidence.aspx. Retrieved 2010-08-10.
- ^ a b c World Health Organization (2003). "Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials". In Zhang X. World Health Organization. http://www.who.int/medicinedocs/en/d/Js4926e/#Js4926e.5.
- ^ a b Sampson, W (2005-03-23). "Critique of the NIH Consensus Conference on Acupuncture". Quackwatch. http://www.acuwatch.org/general/nihcritique.shtml. Retrieved 2009-06-05.
- ^ a b c d McCarthy, Michael (2005). "Critics slam draft WHO report on homoeopathy". The Lancet 366: 705–6. doi:10.1016/S0140-6736(05)67159-0.
- ^ a b Singh & Ernst, 2008, p. 277-8.
- ^ a b c d e f g h Braverman S (2004). "Medical Acupuncture Review: Safety, Efficacy, And Treatment Practices". Medical Acupuncture 15 (3). http://www.medicalacupuncture.org/aama_marf/journal/vol15_3/article1.html.
- ^ a b c Furlan, Andrea D.; Van Tulder, Maurits; Cherkin, Dan; Tsukayama, Hiroshi; Lao, Lixing; Koes, Bart; Berman, Brian (2005). "Acupuncture and Dry-Needling for Low Back Pain: An Updated Systematic Review Within the Framework of the Cochrane Collaboration". Spine 30 (8): 944–63. doi:10.1097/01.brs.0000158941.21571.01. PMID 15834340.
- ^ a b Ramey, D; Buell D (2004). "A true history of acupuncture". Focus on Complementary and Alternative Therapies 9 (4): 269–73. doi:0.1211/fact.2004.00244. http://www.visibleholism.com/html/Acupuncture%20&%20Chinese%20Cultures/History%20of%20Acu/20090412/1516.html.
- ^ Tiran, D; Mack S (2000). Complementary therapies for pregnancy and childbirth. Elsevier Health Sciences. pp. 79. ISBN 0702023280.
- ^ e.g. White, A; Ernst E (1999). Acupuncture: a scientific appraisal. Elsevier Health Sciences. pp. 1. ISBN 0750641630.
- ^ a b Chiu, M (1993). Chinese acupuncture and moxibustion. Elsevier Health Sciences. p. 2. ISBN 0443042233. http://books.google.ca/books?id=V5PAB4d5qmgC&pg=PA2.
- ^ Ma, K.-W. (1992). "The roots and development of Chinese acupuncture: from prehistory to early 20th century". Acupuncture in Medicine 10: 92–9. doi:10.1136/aim.10.Suppl.92.
- ^ Robson, T (2004). An Introduction to Complementary Medicine. Allen & Unwin. pp. 90. ISBN 1741140544.
- ^ Epler Jr, D. C. (1980). "Bloodletting in early Chinese medicine and its relation to the origin of acupuncture". Bulletin of the history of medicine 54 (3): 337–367. PMID 6998524.
- ^ Dorfer, L; Moser, M; Bahr, F; Spindler, K; Egartervigl, E; Giullen, S; Dohr, G; Kenner, T (1999). "A medical report from the stone age?". The Lancet 354: 1023–5. doi:10.1016/S0140-6736(98)12242-0. PMID 10501382. http://www.utexas.edu/courses/classicalarch/readings/Iceman_Tattoos.pdf.
- ^ Barnes, 2005, p. 25.
- ^ Unschuld, P (1998). Chinese Medicine. Paradigm Publications. pp. 94. ISBN 0912111550.
- ^ Barnes, 2005, pp. 58–9.
- ^ Barnes, 2005, p. 75.
- ^ Barnes, 2005, p. 188.
- ^ Barnes, 2005, pp. 308–9.
- ^ Crozier RC (1968). Traditional medicine in modern China: science, nationalism, and the tensions of cultural change. Cambridge: Harvard University Press.[page needed]
- ^ Taylor, K (2005). Chinese Medicine in Early Communist China, 1945-63: a Medicine of Revolution. RoutledgeCurzon. ISBN 041534512X.
- ^ a b Beyerstein, BL; Sampson W (1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 1)". Skeptical Inquirer (Committee for Skeptical Inquiry) 20 (4). http://www.csicop.org/si/show/china_conference_1/.
- ^ Davidson JP (1999). The complete idiot's guide to managing stress. Indianapolis, Ind: Alpha Books. pp. 255. ISBN 0-02-862955-8.
- ^ Frum, David (2000). How We Got Here: The '70s. New York, New York: Basic Books. p. 133. ISBN 0465041957.
- ^ Simon Singh (2006-03-26). "A groundbreaking experiment ... or a sensationalized TV stunt?". The Guardian. http://www.guardian.co.uk/media/2006/mar/25/science.broadcasting.
- ^ Simon Singh (14 February 2006). "Did we really witness the 'amazing power' of acupuncture?". Daily Telegraph. http://www.telegraph.co.uk/science/science-news/3344833/Did-we-really-witness-the-amazing-power-of-acupuncture.html.
- ^ a b Aung & Chen, 2007, pp 11-12.
- ^ "氣的生理功能...(一)推動作用...(二)溫煦作用...(三)防御作用...(四)固攝作用...(五)氣化作用 [Physiological functions of qi ... 1.) Function of actuation ... 2.) Function of warming ... 3.) Function of defense ... 4.) Function of containment ... 5.) Function of transformation ...] as seen at 郭卜樂 (24t October 2009). "氣 [Qi]" (in Chinese). Archived from the original on January 8, 2009. http://web.archive.org/web/20090108191112/http://www.zgxl.net/sljk/imgbody/zyrt/qi.htm. Retrieved 2 December 2010.
- ^ "(三)十二经脉 ...(四)奇经八脉 ..." [(3.) The Twelve Vessels ... (4.) The Extraordinary Eight Vessels ...] as seen at "经络学 [meridian theory]" (in Chinese). http://www.pharmnet.com.cn/tcm/knowledge/detail/100044.html. Retrieved 22 February 2011.
- ^ Aung & Chen, 2007, pp 19-20.
- ^ Needham & Lu, 2002, p. 23.
- ^ Aung & Chen, 2007, p. 101.
- ^ Needham & Lu, 2002, p. 15.
- ^ Wiseman & Ellis 1996, p. 77
- ^ Ergil, MC; Ergil, KV (2009). Pocket Atlas of Chinese Medicine. Stuttgart: Thieme. pp. 19, 148. ISBN 978-3-13-141611-7.
- ^ Flaws, B; Finney D (2007). A handbook of TCM patterns & their treatments (6th ed.). Blue Poppy Press. pp. 1. ISBN 978-0-936185-70-5.
- ^ Flaws; Finney, D (1996). A handbook of TCM patterns & their treatments (6 (2007) ed.). Blue Poppy Press. pp. 169–173. ISBN 978-0-936185-70-5.
- ^ a b Maciocia, G (1995). Tongue Diagnosis in Chinese Medicine. Eastland Press. ISBN 093961619X.
- ^ Maciocia, G (2005). The Foundations of Chinese Medicine. Churchill Livingstone. ISBN 0443074895.
- ^ Ross, J (1984). Zang Fu, the organ systems of traditional Chinese medicine. Elsevier. pp. 26. ISBN 978-0-443-03482-4.
- ^ anon (1980). Essentials of Chinese Acupuncture (1st ed.). Beijing: Foreign Languages Press. pp. 39–46.
- ^ Cheng, 1987, chapter 12.
- ^ Wright, Thomas; Eisenberg, David (1995). Encounters with Qi: exploring Chinese medicine. New York: Norton. pp. 53–4. ISBN 0-393-31213-5.
- ^ Schwartz, L (2000). "Evidence-Based Medicine And Traditional Chinese Medicine: Not Mutually Exclusive". Medical Acupuncture 12 (1): 38-41. http://www.medicalacupuncture.org/aama_marf/journal/vol12_1/evidence.html.
- ^ a b "What is involved in an Acupuncture & Traditional Chinese Medicine (TCM) Treatment?". acupuncture.com. http://www.acupuncture.com.au/education/theory/thefiveelements.html.
- ^ a b c Young, J (2007). Complementary Medicine For Dummies. John Wiley & Sons. pp. 126–8. ISBN 0470519681.
- ^ a b c Napadow, V.; Kaptchuk, T. J. (2004). "Patient Characteristics for Outpatient Acupuncture in Beijing, China". The Journal of Alternative and Complementary Medicine 10 (3): 565–572. doi:10.1089/1075553041323849. PMID 15253864.
- ^ Xu, X. (2001). "Acupuncture in an outpatient clinic in China: A comparison with the use of acupuncture in North America". Southern medical journal 94 (8): 813–816. PMID 11549194.
- ^ a b Guimarães, S. B. (2007). "Acupuncture in an Outpatient Clinic in Fortaleza, Brazil: Patients' Characteristics and Prevailing Main Complaints" (pdf). The Journal of Alternative and Complementary Medicine 13 (3): 308–310. doi:10.1089/acm.2006.6340. PMID 17480128. http://www.cirurgia.ufc.br/services/art07/14.Acupuncture%20in%20an%20outpatient%20clinic%20in%20Fortaleza.pdf.
- ^ Collinge, William J. (1996). The American Holistic Health Association Complete guide to alternative medicine. New York: Warner Books. ISBN 0-446-67258-0.
- ^ a b c Aung & Chen, 2007, p. 116.
- ^ Ellis, A; Wiseman N; Boss K (1991). Fundamentals of Chinese Acupuncture. Paradigm Publications. pp. 2–3. ISBN 091211133X.
- ^ Aung & Chen, 2007, p. 113.
- ^ a b Ishida, Yasuo (1988). "Acupuncture Today". Southern Medical Journal 81 (7): 885–7. doi:10.1097/00007611-198807000-00019. PMID 3393947.
- ^ a b Flachskampf, F. A.; Gallasch, J.; Gefeller, O.; Gan, J.; Mao, J.; Pfahlberg, A. B.; Wortmann, A.; Klinghammer, L. et al. (2007). "Randomized Trial of Acupuncture to Lower Blood Pressure". Circulation 115 (24): 3121–9. doi:10.1161/CIRCULATIONAHA.106.661140. PMID 17548730.
- ^ Itoh, K; Katsumi, Y; Hirota, S; Kitakoji, H (2006). "Effects of trigger point acupuncture on chronic low back pain in elderly patients—a sham-controlled randomised trial.". Acupuncture in Medicine 24 (1): 5–12. PMID 16618043.
- ^ a b Lewith, G; Field, J; MacHin, D (1983). "Acupuncture compared with placebo in post-herpetic pain". Pain 17 (4): 361–8. doi:10.1016/0304-3959(83)90167-7. PMID 6664681.
- ^ uclm.es
- ^ Aung & Chen, 2007, p. 122.
- ^ Needham & Lu, 2002, pp 170–173.
- ^ "Sonopuncture". Educational Opportunities in Integrative Medicine. The Hunter Press. 2008. p. 34. ISBN 9780977655243.
- ^ Bhagat (2004). Alternative Therapies. pp. 164–165. ISBN 9788180612206.
- ^ "Sonopuncture". American Cancer Society's Guide to complementary and alternative cancer methods. American Cancer Society. 2000. p. 158. ISBN 9780944235249.
- ^ "Cancer Dictionary – Acupuncture point injection". National Cancer Institute. http://www.cancer.gov/dictionary?CdrID=467825. Retrieved 2011-04-04.
- ^ Isaacs, Nora (13 December 2007). "Hold the Chemicals, Bring on the Needles". New York Times. http://www.nytimes.com/2007/12/13/fashion/13SKIN.html?pagewanted=1&ref=fashion. Retrieved 23 November 2009.
- ^ Lee, M. S.; Ernst, E. (2011). "Acupuncture for pain: An overview of Cochrane reviews". Chinese Journal of Integrative Medicine 17 (3): 187–189. doi:10.1007/s11655-011-0665-7. PMID 21359919.
- ^ Manheimer E, White A, Berman B, Forys K, Ernst E (2005). "Meta-analysis: acupuncture for low back pain" (PDF). Ann Intern Med 142 (8): 651–63. PMID 15838072. http://www.annals.org/cgi/reprint/142/8/651.pdf.
- ^ PMID 17909210 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ^ a b c O'Connell, NE; Wand, BM; Goldacre, B (2009). "Interpretive bias in acupuncture research?: A case study.". Evaluation & the health professions 32 (4): 393–409. doi:10.1177/0163278709353394. PMID 19942631.
- ^ Trinh K, Graham N, Gross A, Goldsmith C, Wang E, Cameron I, Kay T (2007). "Acupuncture for neck disorders". Spine 32 (2): 236–43. doi:10.1097/01.brs.0000252100.61002.d4. PMID 17224820.; Trinh K, Graham N, Gross A, Goldsmith C, Wang E, Cameron I, Kay T (2006). Trinh, Kien. ed. "Acupuncture for neck disorders". Cochrane Database of Systematic Reviews 3: CD004870. doi:10.1002/14651858.CD004870.pub3. PMID 16856065. http://www.cochrane.org/reviews/en/ab004870.html.
- ^ Melchart, D; Linde, K; Fischer, P; Berman, B; White, A; Vickers, A; Allais, G (2001). Melchart, Dieter. ed. "Acupuncture for idiopathic headache.". Cochrane Database of Systematic Reviews (Online) (1): CD001218. doi:10.1002/14651858.CD001218. PMID 11279710.
- ^ Linde, K; Allais, G; Brinkhaus, B; Manheimer, E; Vickers, A; White, AR (2009). Linde, Klaus. ed. "Acupuncture for migraine prophylaxis.". Cochrane Database of Systematic Reviews (Online) (1): CD001218. doi:10.1002/14651858.CD001218.pub2. PMC 3099267. PMID 19160193. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3099267.
- ^ White A, Foster NE, Cummings M, Barlas P (2007). "Acupuncture treatment for chronic knee pain: a systematic review". Rheumatology 46 (3): 384–90. doi:10.1093/rheumatology/kel413. PMID 17215263.
- ^ Selfe TK, Taylor AG (2008 Jul–Sep). "Acupuncture and osteoarthritis of the knee: a review of randomized, controlled trials". Fam Community Health 31 (3): 247–54. doi:10.1097/01.FCH.0000324482.78577.0f (inactive 2009-11-14). PMC 2810544. PMID 18552606. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2810544.
- ^ a b Manheimer, E; Linde, K; Lao, L; Bouter, LM; Berman, BM (2007). "Meta-analysis: acupuncture for osteoarthritis of the knee.". Annals of internal medicine 146 (12): 868–77. PMID 17577006.
- ^ Zhang, W; Moskowitz, RW; Nuki, G; Abramson, S; Altman, RD; Arden, N; Bierma-Zeinstra, S; Brandt, KD et al. (2008). "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines" (pdf). Osteoarthritis and Cartilage 16 (2): 137–162. doi:10.1016/j.joca.2007.12.013. PMID 18279766. http://www.oarsi.org/pdfs/oarsi_recommendations_for_management_of_hip_and_knee_oa.pdf.
- ^ Manheimer, E.; Cheng, K.; Linde, K.; Lao, L.; Yoo, J.; Wieland, S.; Van Der Windt, D. L. A. M.; Berman, B. M. et al. (2010). Acupuncture for peripheral joint osteoarthritis. In Manheimer, Eric. "Acupuncture for peripheral joint osteoarthritis". Cochrane database of systematic reviews (Online) (1): CD001977. doi:10.1002/14651858.CD001977.pub2. PMC 3169099. PMID 20091527. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3169099.
- ^ Lee A, Done ML (2004). Lee, Anna. ed. "Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting". Cochrane Database of Systematic Reviews (Online) (3): CD003281. doi:10.1002/14651858.CD003281.pub2. PMID 15266478. http://www.cochrane.org/reviews/en/ab003281.html.
- ^ Ezzo, JM; Richardson, MA; Vickers, A; Allen, C; Dibble, SL; Issell, BF; Lao, L; Pearl, M et al. (2006). Ezzo, Jeanette. ed. "Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting". Cochrane Database of Systematic Reviews (Online) (2): CD002285. doi:10.1002/14651858.CD002285.pub2. PMID 16625560. http://www.cochrane.org/reviews/en/ab002285.html.
- ^ Isaacs, Lyndsey; West, Zita (2008). Acupuncture in pregnancy and childbirth. Philadelphia: Churchill Livingstone/Elsevier. ISBN 0-443-10371-2. http://books.google.ca/books?id=BhVvDfLypxIC&printsec=frontcover#v=onepage&q&f=false.
- ^ Cheong, Y. C.; Hung Yu Ng, E.; Ledger, W. L. (2008). Acupuncture and assisted conception. In Cheong, Ying C. "Cochrane Database of Systematic Reviews". Cochrane database of systematic reviews (Online) (4): CD006920. doi:10.1002/14651858.CD006920.pub2. PMID 18843737.
- ^ El-Toukhy, T.; Khalaf, Y. (2009). "The impact of acupuncture on assisted reproductive technology outcome". Current Opinion in Obstetrics and Gynecology 21 (3): 240–246. doi:10.1097/GCO.0b013e3283292491. PMID 19276803.
- ^ El-Toukhy, T.; Khalaf, Y. (2010). "A new study of acupuncture in IVF: Pointing in the right direction". Reproductive BioMedicine Online 21 (3): 278–279. doi:10.1016/j.rbmo.2010.06.024. PMID 20650689.
- ^ "Cochrane and Alternative Medicine - Acupuncture". Danish Knowledge and Research Center for Alternative Medicines. 2011-09-28. http://www.vifab.dk/uk/cochrane+and+alternative+medicine/acupuncture?. Retrieved 2011-10-19.
- ^ McCarney, RW; Brinkhaus, B; Lasserson, TJ; Linde, K; McCarney, Robert W (2003). McCarney, Robert W. ed. "Acupuncture for chronic asthma". Cochrane Database of Systematic Reviews 2003 (3): CD000008. doi:10.1002/14651858.CD000008.pub2. PMID 14973944. http://www.cochrane.org/reviews/en/ab000008.html. Retrieved 2008-05-02.
- ^ He, L; Zhou, MK; Zhou, D; Wu, B; Li, N; Kong, SY; Zhang, DP; Li, QF et al. (2004). He, Li. ed. "Acupuncture for Bell's palsy". Cochrane Database of Systematic Reviews 2007 (4): CD002914. doi:10.1002/14651858.CD002914.pub3. PMID 17943775. http://www.cochrane.org/reviews/en/ab002914.html. Retrieved 2008-05-02.
- ^ Gates, S; Smith, LA; Foxcroft, DR; Gates, Simon (2006). Gates, Simon. ed. "Auricular acupuncture for cocaine dependence". Cochrane Database of Systematic Reviews 2006 (1): CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523. http://www.cochrane.org/reviews/en/ab005192.html. Retrieved 2008-05-02.
- ^ Smith, CA; Hay, PP; Smith, Caroline A (2004-03-17). Smith, Caroline A. ed. "Acupuncture for depression". Cochrane Database of Systematic Reviews 2004 (3): CD004046. doi:10.1002/14651858.CD004046.pub2. PMID 15846693. http://www.cochrane.org/reviews/en/ab004046.html. Retrieved 2008-05-02.
- ^ Jordan, J (2006). "Acupuncture treatment for opiate addiction: A systematic review". Journal of Substance Abuse Treatment 30 (4): 309–14. doi:10.1016/j.jsat.2006.02.005. PMID 16716845.
- ^ Gates, Simon; Smith, Lesley A; Foxcroft, David (2006). Gates, Simon. ed. Auricular acupuncture for cocaine dependence. pp. CD005192. doi:10.1002/14651858.CD005192.pub2. PMID 16437523.
- ^ Bearn, Jennifer; Swami, Anshul; Stewart, Duncan; Atnas, Catherine; Giotto, Lisa; Gossop, Michael (2009). "Auricular acupuncture as an adjunct to opiate detoxification treatment: Effects on withdrawal symptoms". Journal of Substance Abuse Treatment 36 (3): 345–9. doi:10.1016/j.jsat.2008.08.002. PMID 19004596.
- ^ Proctor, ML; Smith, CA; Farquhar, CM; Stones, RW; Zhu, Xiaoshu; Brown, Julie; Zhu, Xiaoshu (2002). Zhu, Xiaoshu. ed. "Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea". Cochrane Database of Systematic Reviews 2002 (1): CD002123. doi:10.1002/14651858.CD002123. PMID 11869624. http://www.cochrane.org/reviews/en/ab002123.html. Retrieved 2008-05-02.
- ^ Cheuk, DK; Wong, V; Cheuk, Daniel (2006). Cheuk, Daniel. ed. "Acupuncture for epilepsy". Cochrane Database of Systematic Reviews 2006 (2): CD005062. doi:10.1002/14651858.CD005062.pub2. PMID 16625622. http://www.cochrane.org/reviews/en/ab005062.html. Retrieved 2008-05-02.
- ^ Mayhew E; Ernst E (2007). "Acupuncture for fibromyalgia—a systematic review of randomized clinical trials". Rheumatology (Oxford, England) 46 (5): 801–4. doi:10.1093/rheumatology/kel406. PMID 17189243.
- ^ Law, SK; Li, T; Law, Simon K (2007). Law, Simon K. ed. "Acupuncture for glaucoma". Cochrane Database of Systematic Reviews 2007 (4): CD006030. doi:10.1002/14651858.CD006030.pub2. PMID 17943876. http://www.cochrane.org/reviews/en/ab006030.html. Retrieved 2008-05-02.
- ^ Cheuk, DK; Yeung, WF; Chung, KF; Wong, V; Cheuk, Daniel KL (2007). Cheuk, Daniel KL. ed. "Acupuncture for insomnia". Cochrane Database of Systematic Reviews 2007 (3): CD005472. doi:10.1002/14651858.CD005472.pub2. PMID 17636800. http://www.cochrane.org/reviews/en/ab005472.html. Retrieved 2008-05-02.
- ^ Lim, B; Manheimer, E; Lao, L; Ziea, E; Wisniewski, J; Liu, J; Berman, B; Manheimer, Eric (2006). Manheimer, Eric. ed. "Acupuncture for treatment of irritable bowel syndrome". Cochrane Database of Systematic Reviews 2006 (4): CD005111. doi:10.1002/14651858.CD005111.pub2. PMID 17054239. http://www.cochrane.org/reviews/en/ab005111.html. Retrieved 2008-05-06.
- ^ Smith, CA; Crowther, CA; Smith, Caroline A (2004). Smith, Caroline A. ed. "Acupuncture for induction of labour". Cochrane Database of Systematic Reviews 2004 (1): CD002962. doi:10.1002/14651858.CD002962.pub2. PMID 14973999. http://www.cochrane.org/reviews/en/ab002962.html. Retrieved 2008-05-06.
- ^ Casimiro, L; Barnsley, L; Brosseau, L; Milne, S; Robinson, VA; Tugwell, P; Wells, G; Casimiro, Lynn (2005). Casimiro, Lynn. ed. "Acupuncture and electroacupuncture for the treatment of rheumatoid arthritis". Cochrane Database of Systematic Reviews 2005 (4): CD003788. doi:10.1002/14651858.CD003788.pub2. PMID 16235342. http://www.cochrane.org/reviews/en/ab003788.html. Retrieved 2008-05-06.
- ^ Green, S; Buchbinder, R; Hetrick, S; Green, Sally (2005). Green, Sally. ed. "Acupuncture for shoulder pain". Cochrane Database of Systematic Reviews 2005 (2): CD005319. doi:10.1002/14651858.CD005319. PMID 15846753. http://www.cochrane.org/reviews/en/ab005319.html. Retrieved 2008-05-06.
- ^ Rathbone, J; Xia, J; Rathbone, John (2005). Rathbone, John. ed. "Acupuncture for schizophrenia". Cochrane Database of Systematic Reviews 2005 (4): CD005475. doi:10.1002/14651858.CD005475. PMID 16235404. http://www.cochrane.org/reviews/en/ab005475.html. Retrieved 2008-05-06.
- ^ White, AR; Rampes, H; Campbell, JL; White, Adrian R (2006). White, Adrian R. ed. "Acupuncture and related interventions for smoking cessation". Cochrane Database of Systematic Reviews 2006 (1): CD000009. doi:10.1002/14651858.CD000009.pub2. PMID 16437420. http://www.cochrane.org/reviews/en/ab000009.html. Retrieved 2008-05-06.
- ^ Zhang, SH; Liu, M; Asplund, K; Li, L; Liu, Ming (2005). Liu, Ming. ed. "Acupuncture for acute stroke". Cochrane Database of Systematic Reviews 2005 (2): CD003317. doi:10.1002/14651858.CD003317.pub2. PMID 15846657. http://www.cochrane.org/reviews/en/ab003317.html. Retrieved 2008-05-06.
- ^ Wu, HM; Tang, JL; Lin, XP; Lau, J; Leung, PC; Woo, J; Li, YP; Wu, Hong Mei (2006). Wu, Hong Mei. ed. "Acupuncture for stroke rehabilitation". Cochrane Database of Systematic Reviews 2006 (3): CD004131. doi:10.1002/14651858.CD004131.pub2. PMID 16856031. http://www.cochrane.org/reviews/en/ab004131.html. Retrieved 2008-05-06.
- ^ Green, S; Buchbinder, R; Barnsley, L; Hall, S; White, M; Smidt, N; Assendelft, W; Green, Sally (2002). Green, Sally. ed. "Acupuncture for lateral elbow pain". Cochrane Database of Systematic Reviews 2002 (1): CD003527. doi:10.1002/14651858.CD003527. PMID 11869671. http://www.cochrane.org/reviews/en/ab003527.html. Retrieved 2008-05-06.
- ^ Peng, WN; Zhao, H; Liu, ZS; Wang, S; Weina, Peng (2008). Weina, Peng. ed. "Acupuncture for vascular dementia". Cochrane Database of Systematic Reviews 2007 (2): CD004987. doi:10.1002/14651858.CD004987.pub2. PMID 17443563. http://www.cochrane.org/reviews/en/ab004987.html. Retrieved 2008-05-06.
- ^ Napadow, Vitaly; Ahn, Andrew; Longhurst, John; Lao, Lixing; Stener-Victorin, Elisabet; Harris, Richard; Langevin, Helene M. (2008). "The Status and Future of Acupuncture Mechanism Research". The Journal of Alternative and Complementary Medicine 14 (7): 861–9. doi:10.1089/acm.2008.SAR-3. PMID 18803495.
- ^ Vickers, A.; Goyal, N.; Harland, R.; Rees, R. (1998). "Do certain countries produce only positive results? A systematic review of controlled trials" (pdf). Controlled clinical trials 19 (2): 159–166. PMID 9551280. http://www.dcscience.net/Vickers_1998_Controlled-Clinical-Trials.pdf.
- ^ "Position Paper on Acupuncture". National Council Against Health Fraud. 1990. http://www.ncahf.org/pp/acu.html. Retrieved 2011-01-27.
- ^ Arthur Taub (1993). Acupuncture: Nonsense with Needles. http://www.acuwatch.org/general/taub.shtml.
- ^ Stephen Barrett, M.D.. "Be Wary of Acupuncture, Qigong, and "Chinese Medicine"". http://www.quackwatch.org/01QuackeryRelatedTopics/acu.html. Retrieved 2010-05-31.
- ^ John P. Jackson. "What is acupuncture?". http://www.ukskeptics.com/acupuncture.php.
- ^ Steven Salzberg (2008). "Acupuncture infiltrates the University of Maryland and NEJM". http://genome.fieldofscience.com/2010/08/acupuncture-infiltrates-university-of.html.
- ^ Steven Novella. "Acupuncture Pseudoscience in the New England Journal of Medicine". http://www.sciencebasedmedicine.org/?p=6391.
- ^ Sampson WI (2005). "Critique of the NIH Consensus Conference on Acupuncture". Acuwatch. http://www.acuwatch.org/general/nihcritique.shtml.
- ^ Sampson WI, Atwood K (5/19 December 2005). "Propagation of the Absurd: demarcation of the Absurd revisited". Med J Aust 183 (11/12): Viewpoint. https://www.mja.com.au/public/issues/183_11_051205/sam10986_fm.pdf.
- ^ Acupuncture, American Cancer Society
- ^ Becker, Robert O.; Selden, Gary (1985). The Body Electric. New York: William Morrow. ISBN 0-688-06971-1.
- ^ Colbert, A. P.; Spaulding, K.; Larsen, A.; Ahn, A. C.; Cutro, J. A. (2011). "Electrodermal Activity at Acupoints: Literature Review and Recommendations for Reporting Clinical Trials". Journal of Acupuncture and Meridian Studies 4 (1): 5–13. doi:10.1016/S2005-2901(11)60002-2. PMID 21440875.
- ^ Mann, Felix (2000). Reinventing acupuncture: a new concept of ancient medicine. Oxford: Butterworth-Heinemann. pp. 14; 31. ISBN 0-7506-4857-0. OCLC 44162535.
- ^ Kalichman, L.; Vulfsons, S. (2010). "Dry Needling in the Management of Musculoskeletal Pain". The Journal of the American Board of Family Medicine 23: 640–6. doi:10.3122/jabfm.2010.05.090296.
- ^ Traditional Chinese Medicine
- ^ Sampson, WI (September/October 1996). "Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 2)". Skeptical Inquirer 20 (5). http://www.csicop.org/si/show/china_conference_2/. Retrieved 2009-09-26.
- ^ Sun, Y.; Gan, T. J.; Dubose, J. W.; Habib, A. S. (2008). "Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials". British Journal of Anaesthesia 101 (2): 151–60. doi:10.1093/bja/aen146. PMID 18522936.
- ^ "Report 12 of the Council on Scientific Affairs (A-97) – Alternative Medicine". American Medical Association. 1997. http://www.ama-assn.org/ama/no-index/about-ama/13638.shtml. Retrieved 2009-10-07.
- ^ Norheim, Arne Johan (1996). "Adverse Effects of Acupuncture: A Study of the Literature for the Years 1981–1994". The Journal of Alternative and Complementary Medicine 2 (2): 291–7. doi:10.1089/acm.1996.2.291. PMID 9395661.
- ^ a b Woo, P. C Y; Lin, A. W C; Lau, S. K P; Yuen, K.-Y. (2010). "Acupuncture transmitted infections". BMJ 340: c1268. doi:10.1136/bmj.c1268. PMID 20299695. http://www.bmj.com/content/340/bmj.c1268.full.
- ^ White, A.; Hayhoe, S.; Hart, A.; Ernst, E. (2001). "Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists". BMJ 323 (7311): 485–6. doi:10.1136/bmj.323.7311.485. PMC 48133. PMID 11532840. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=48133.
- ^ Ernst, E (2010). "Deaths after acupuncture: A systematic review". The International Journal of Risk and Safety in Medicine 22 (3): 131–6. doi:10.3233/JRS-2010-0503.
- ^ Leavy, Benjamin R. (2002). "Apparent adverse outcome of acupuncture.". The Journal of the American Board of Family Practice / American Board of Family Practice 15 (3): 246–8. PMID 12038734. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=12038734.
- ^ Leow TK (2001). "Pneumothorax Using Bladder 14". Medical Acupuncture 16 (2). http://www.medicalacupuncture.org/aama_marf/journal/vol16_2/case_2.html.
- ^ Yekeler, E.; Tunaci, M; Tunaci, A; Dursun, M; Acunas, G (2006). "Frequency of Sternal Variations and Anomalies Evaluated by MDCT". American Journal of Roentgenology 186 (4): 956–60. doi:10.2214/AJR.04.1779. PMID 16554563. http://www.ajronline.org/content/186/4/956.full.
- ^ Barret, S (2007-12-30). "Be Wary of Acupuncture, Qigong, and "Chinese Medicine"". Quackwatch. http://www.quackwatch.org/01QuackeryRelatedTopics/acu.html. Retrieved 2010-11-03.
- ^ "Final Report, Report into Traditional Chinese Medicine" (pdf). Parliament of New South Wales. 2005-11-09. http://www.parliament.nsw.gov.au/prod/parlment/committee.nsf/0/ca78e168ce1b6fa2ca2570b400200a34/$FILE/reportversion2.pdf. Retrieved 2010-11-03.
- ^ "NCCAOM Code of Ethics" (pdf). National Certification Commission for Acupuncture and Oriental Medicine. http://www.nccaom.org/about/pdfdocs/Code_of_Ethics.pdf. Retrieved 2010-11-03.
- ^ "Traditional Chinese Medicine Act, 2006". ServiceOntario. 2007-06-04. http://www.search.e-laws.gov.on.ca/en/isysquery/f810a2e9-6cd9-42ff-926d-4de171f932ee/1/doc/?search=browseStatutes&context=#hit1. Retrieved 2010-11-03.[dead link]
- ^ "Health Professions Act: Traditional Chinese Medicine Practitioners and Acupuncturists Regulation". Queen’s Printer for British Columbia. 2008-10-15. http://www.bclaws.ca/EPLibraries/bclaws_new/document/ID/freeside/32_290_2008. Retrieved 2010-11-03.
- ^ nccaom.org
- ^ State Licensure Table
- ^ "Physicians Divided on Impact of CAM on U.S. Health Care; Aromatherapy Fares Poorly; Acupuncture Touted". HCD Research. 9 September 2005. Archived from the original on 2006-01-10. http://web.archive.org/web/20060110033955/http://publish.hcdhealth.com/P1007/CumulativeReport.htm. "More than half of the physicians (59%) believed that acupuncture can be effective to some extent."
- ^ Updates-June 1996 FDA Consumer
- ^ US FDA/CDRH: Premarket Approvals
- ^ Report: Insurance Coverage for Acupuncture on the Rise. Michael Devitt, Acupuncture Today, January, 2005, Vol. 06, Issue 01
- ^ Claxton, Gary; Isadora Gil, Ben Finder, Erin Holve, Jon Gabel, Jeremy Pickreighn, Heidi Whitmore, Samantha Hawkins, and Cheryl Fahlman (2004). The Kaiser Family Foundation and Health Research and Educational Trust Employer Health Benefits 2004 Annual Survey. Kaiser Family Foundation. pp. 106–7. ISBN 0-87258-812-2. http://www.kff.org/insurance/7148/upload/2004-Employer-Health-Benefits-Survey-Full-Report.pdf.
- ^ "Traditional Chinese Medicine Act, 2006". S.O. 2006, c. 27. http://www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_06t27_e.htm.
- ^ "What is the TC-CTCMPAO?". College of Traditional Chinese Medicine Practitioners and Acupuncturists of Ontario. http://www.ctcmpao.on.ca/index.html. Retrieved 2009-09-02.
- ^ "British Acupuncture Council". http://www.acupuncture.org.uk/index.php.
- ^ "The British Medical Acupuncture Society". http://www.medical-acupuncture.co.uk.
- ^ "Acupuncture Association of Chartered Physiotherapists". http://www.aacp.org.uk.
- ^ http://www.ahpra.gov.au/
- ^ "Welcome to the Chinese Medicine Registration Board of Victoria". http://www.cmrb.vic.gov.au.
- ^ "Health NSW" (PDF). http://www.health.nsw.gov.au/public-health/ehb/general/skinpen/skin_pen_reg_2000.pdf.
- ^ "Scopes of Practice". osteopathiccouncil.org.nz. http://www.osteopathiccouncil.org.nz/scopes-of-practice.html.
- ^ "ACC Releases Guidelines for Acupuncture Treatment". Accident Compensation Corporation. http://www.acc.co.nz/news/WIM2_059369.
Further reading
- Deadman, P; Baker K; Al-Khafaji M (2007). A Manual of Acupuncture. Journal of Chinese Medicine Publications. ISBN 0951054651.
- Jin, G; Jin JX; Jin LL (2006). Contemporary Medical Acupuncture – A Systems Approach (English). Springer. ISBN 7040192578. http://books.google.com/?id=OaMHyVg5nNcC&printsec=frontcover&q=.
External links
TCM Practices 
Three Treasures (Sānbǎo 三寶) Other Key TCM Topics Yin Entities (Zàng 臟) Heart · Kidney · Pericardium · Liver · Lung · SpleenYang Entities (Fǔ 腑) Gallbladder · Large Intestine · Small Intestine · Stomach · Triple Warmer (Sānjiaō) · Urinary BladderFamous TCM Physicians Hua Tuo 华陀 (141-208) · Li Shizhen 李时珍 (1518-1593) · Sun Simiao 孙思邈 (540–682) · Zhang Jiegu (ca. 1151-1234) · Zhang Zhongjing 張仲景 (150-219)Contemporary Related Topics Category · PortalAcupuncture Concepts Types Category · PortalCategories:- Acupuncture
- Chinese inventions
- Energy therapies
- Alternative medicine
Wikimedia Foundation. 2010.