- Acne vulgaris
-
This article is about a skin disease commonly found during adolescence. For other acneform skin diseases, see Acne (disambiguation).
Acne vulgaris Classification and external resources 
Acne of a 14-year-old male during pubertyICD-10 L70.0 ICD-9 706.1 DiseasesDB 10765 MedlinePlus 000873 eMedicine derm/2 MeSH D000152 Acne vulgaris (or cystic acne) is a common human skin disease, characterized by areas of skin with seborrhea (scaly red skin), comedones (blackheads and whiteheads), papules (pinheads), pustules (pimples), Nodules (large papules) and possibly scarring.[1] Acne affects mostly skin with the densest population of sebaceous follicles; these areas include the face, the upper part of the chest, and the back. Severe acne is inflammatory, but acne can also manifest in noninflammatory forms.[2] The lesions are caused by changes in pilosebaceous units, skin structures consisting of a hair follicle and its associated sebaceous gland, changes that require androgen stimulation.
Acne occurs most commonly during adolescence, and often continues into adulthood. In adolescence, acne is usually caused by an increase in testosterone, which people of both genders accrue during puberty.[3] For most people, acne diminishes over time and tends to disappear — or at the very least decrease — after one reaches one's early twenties. There is, however, no way to predict how long it will take to disappear entirely, and some individuals will carry this condition well into their thirties, forties, and beyond.[4]
Some of the large nodules were previously called "cysts" and the term nodulocystic has been used to describe severe cases of inflammatory acne.[5] The "cysts," or boils that accompany cystic acne, can appear on the buttocks, groin, and armpit area, and anywhere else where sweat collects in hair follicles and perspiration ducts.[6] Cystic acne affects deeper skin tissue than does common acne.[7]
Aside from scarring, its main effects are psychological, such as reduced self-esteem[8] and in very extreme cases, depression or suicide.[9] Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated by some to lessen the overall long-term impact to individuals.[8]
Contents
Terminology
The term acne comes from a corruption of the Greek ἀκμή (akmē), literally "point, edge", but in the sense of a "skin eruption"[10] in the writings of Aëtius Amidenus. Used by itself, the term "acne" refers to the presence of pustules and papules.[11] The most common form of acne is known as acne vulgaris, meaning "common acne". Many teenagers get this type of acne. Use of the term "acne vulgaris" implies the presence of comedones.[12]
The term "acne rosea" is a synonym for rosacea, however some individuals may have almost no acne comedones associated with their rosacea and prefer therefore the term rosacea.[13] Chloracne is associated with exposure to polyhalogenated compounds.
Signs and symptoms
Typical features of acne include: seborrhea (scaly red skin), comedones (blackheads and whiteheads), papules (pinheads), pustules (pimples), nodules (large papules) and, possibly scarring.[1] It presents somewhat differently in people with dark skin.
Scars
Acne scars are the result of inflammation within the dermis brought on by acne. The scar is created by the wound trying to heal itself resulting in too much collagen in one spot.[14]
Physical acne scars are often referred to as "Icepick" scars. This is because the scars tend to cause an indentation in the skin's surface. There are a range of treatments available. Although quite rare, the medical condition Atrophia Maculosa Varioliformis Cutis also results in "acne-like" depressed scars on the face.
- Ice pick scars: Deep pits, that are the most common and a classic sign of acne scarring.
- Box car scars: Angular scars that usually occur on the temple and cheeks, and can be either superficial or deep, these are similar to chickenpox scars.
- Rolling scars: Scars that give the skin a wave-like appearance.
- Hypertrophic scars: Thickened, or keloid scars.
Pigmentation
Pigmented scars is a slightly misleading term, as it suggests a change in the skin's pigmentation and that they are true scars; however, neither is true. Pigmented scars are usually the result of nodular or cystic acne (the painful 'bumps' lying under the skin). They often leave behind an inflamed red mark. Often, the pigmentation scars can be avoided simply by avoiding aggravation of the nodule or cyst. Pigmentation scars nearly always fade with time taking between three months to two years to do so, although can last forever if untreated.
Cause
Acne develops as a result of blockages in follicles. Hyperkeratinization and formation of a plug of keratin and sebum (a microcomedo) is the earliest change. Enlargement of sebaceous glands and an increase in sebum production occur with increased androgen (DHEA-S) production at adrenarche. The microcomedo may enlarge to form an open comedone (blackhead) or closed comedone (milia). Comedones are the direct result of sebaceous glands' becoming clogged with sebum, a naturally occurring oil, and dead skin cells. In these conditions, the naturally occurring largely commensal bacterium Propionibacterium acnes can cause inflammation, leading to inflammatory lesions (papules, infected pustules, or nodules) in the dermis around the microcomedo or comedone, which results in redness and may result in scarring or hyperpigmentation.[15]
Hormonal
Hormonal activity, such as menstrual cycles and puberty, may contribute to the formation of acne. During puberty, an increase in male sex hormones called androgens cause the follicular glands to grow larger and make more sebum.[16] Use of anabolic steroids may have a similar effect.[17] Several hormones have been linked to acne: the androgens testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), as well as insulin-like growth factor 1 (IGF-I).
Development of acne vulgaris in later years is uncommon, although this is the age group for rosacea, which may have similar appearances. True acne vulgaris in adult women may be a feature of an underlying condition such as pregnancy and disorders such as polycystic ovary syndrome or the rare Cushing's syndrome. Menopause-associated acne occurs as production of the natural anti-acne ovarian hormone estradiol fails at menopause. The lack of estradiol also causes thinning hair, hot flushes, thin skin, wrinkles, vaginal dryness, and predisposes to osteopenia and osteoporosis as well as triggering acne (known as acne climacterica in this situation).
Genetic
The tendency to develop acne runs in families. For example, school aged boys with acne often have other members in their family with acne. A family history of acne is associated with an earlier occurrence of acne and an increased number of retentional acne lesions.[18]
Psychological
While the connection between acne and stress has been debated, scientific research indicates that "increased acne severity" is "significantly associated with increased stress levels."[19] The National Institutes of Health (USA) list stress as a factor that "can cause an acne flare."[20] A study of adolescents in Singapore "observed a statistically significant positive correlation […] between stress levels and severity of acne."[21] It is also not clear whether acne causes stress and thus perpetuates itself to some extent.
Infectious
Propionibacterium acnes (P. acnes) is the anaerobic bacterium species that is widely concluded to cause acne, though Staphylococcus epidermidis has been universally discovered to play some role since normal pores appear colonized only by P.acnes.[22] Regardless, there are specific clonal sub-strains of P.acnes associated with normal skin health and others with long-term acne problems. It is as yet inconclusive whether any of these undesirable strains evolve on-site in the adverse conditions or are all pathogenically acquired, or possibly either depending on the individual patient. These strains either have the capability of changing, perpetuating, or adapting to, the abnormal cycle of inflammation, oil production, and inadequate sloughing activities of acne pores. At least one particularly virulent strain, though, has been circulating around Europe for at least 87 years. [23]In vitro, resistance of P. acnes to commonly used antibiotics has been increasing, as well.[24]
Diet
A high glycemic load diet is associated with worsening acne.[25] There is also an association between the consumption of milk and the rate and severity of acne.[25][26] Other associations such as chocolate and salt are not supported by the evidence.[25] However, products with these ingredients often contain a high glycemic load.
Diagnosis
There are multiple grading scales for grading the severity of acne vulgaris,[27] three of these being:
- Leeds acne grading technique: Counts and categorises lesions into inflammatory and non-inflammatory (ranges from 0–10.0).
- Cook's acne grading scale: Uses photographs to grade severity from 0 to 8 (0 being the least severe and 8 being the most severe).
- Pillsbury scale: Simply classifies the severity of the acne from 1 (least severe) to 4 (most severe).
Differential
Management
Many different treatments exist for acne including benzoyl peroxide, antibiotics, retinoids, antiseborrheic medications, anti-androgen medications, hormonal treatments, salicylic acid, alpha hydroxy acid, azelaic acid, nicotinamide, and keratolytic soaps.[28] They are believed to work in at least 4 different ways, including: normalising shedding into the pore to prevent blockage, killing Propionibacterium acnes, anti-inflammatory effects, hormonal manipulation.[citation needed]
Exercise
Increased blood flow following exercise assists the maintenance of skin cells as it brings in oxygen and nutrients while removing waste. A secondary effect of exercise on acne is that it can reduce stress. [29]
Medications
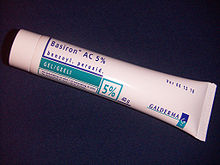
- Benzoyl peroxide
Benzoyl peroxide is a first-line treatment for mild and moderate acne vulgaris due to its effectiveness and mild side-effects (primarily an irritant dermatitis). It works against the "P. acnes" bacterium, and normally causes just dryness of the skin, slight redness, and occasional peeling when side-effects occur.[30] This topical does increase sensitivity to the sun as indicated on the package, so sunscreen should be used during the treatment to prevent sunburn. Benzoyl peroxide has been found to be nearly as effective as antibiotics with all concentrations 2.5%, 5.0%, and 10% equally effective.[30] Unlike antibiotics, benzoyl peroxide does not appear to generate bacterial resistance.[30]
- Antibiotics
Antibiotics are reserved for more severe cases.[30] With increasing resistance of P. acnes worldwide, they are becoming less effective.[30] Commonly used antibiotics, either applied topically or taken orally, include erythromycin, clindamycin, and tetracyclines such as minocycline.
- Hormones
In females, acne can be improved with hormonal treatments. The common combined estrogen/progestogen methods of hormonal contraception have some effect, but the antiandrogen cyproterone in combination with an oestrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side-effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case. Along with this, treatment with low-dose spironolactone can have anti-androgenetic properties, especially in patients with polycystic ovarian syndrome.
- Topical retinoids
A group of medications for normalizing the follicle cell life-cycle are topical retinoids such as tretinoin (Retin-A), adapalene (Differin), and tazarotene (Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and, in general, have much milder side-effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death life-cycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar, but milder, effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use for over 30 years, but are available only on prescription, so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare-up of acne and facial flushing.
- Oral retinoids
A daily oral intake of vitamin A derivative isotretinoin (marketed as Roaccutane, Accutane, Amnesteem, Sotret, Claravis, Clarus) over a period of 4–6 months can cause long-term resolution or reduction of acne. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affects other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side-effects (many of which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4–6 months may be indicated to obtain desired results. It is often recommended that one let a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also gives the body a chance to recover. On occasion, a third or even a fourth course is used, but the benefits are often less substantial. The most common side-effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare-up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated or reduced due to elevated liver enzymes in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports[weasel words] suggest that isotretinoin may cause depression, but, as of September 2005, there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given to females as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge program) for use were put into force in the USA beginning in March 2006 to prevent misuse, causing occasioned widespread editorial comment.[31]
- Anti-inflammatories
Nicotinamide, (vitamin B3) used topically in the form of a gel, has been shown in a 1995 study to be of comparable efficacy to topical clindamycin used for comparison.[32] The property of topical nicotinamide's benefit in treating acne seems to be its anti-inflammatory nature. It is also purported to result in increased synthesis of collagen, keratin, involucrin and flaggrin, and may also, according to a cosmetic company, be useful for reducing skin hyperpigmentation (acne scars), increasing skin moisture and reducing fine wrinkles.[33]
Ibuprofen in combination with tetracycline[34] are used for some moderate acne cases for their anti-inflammatory effects.
Mandelic acid has been noted to be an effective topical treatment for mild to moderate acne. It is considered to be a gentler alternative to popular alpha hydroxy acids, such as glycolic acid and lactic acid.[35]
Procedures
Dermabrasion
Dermabrasion is a cosmetic medical procedure in which the surface of the skin is removed by abrasion (sanding). It is used to remove sun-damaged skin and to remove or lessen scars and dark spots on the skin. The procedure is very painful and usually requires a general anaesthetic or "twilight anaesthesia", in which the patient is still partly conscious.[4] Afterward, the skin is very red and raw-looking, and it takes several months for the skin to regrow and heal. Dermabrasion is useful for scar removal when the scar is raised above the surrounding skin, but is less effective with sunken scars.
In the past, dermabrasion was done using a small, sterilized, electric sander. In the past decade, it has become more common to use laser dermabrasion using CO2, Er:YAG laser or a combination of both for the treatment of acne scars. Indications for CO2 laser treatment include previous non erythematous and non-proliferative hypertrophic scars, atrophic acne scars and burn scars.[36] Laser dermabrasion is much easier to control, much easier to gauge, and is practically bloodless compared to classic dermabrasion.
Phototherapy
Blue and red light
Light exposure has long been used as a short-term treatment for acne. Recently, visible light has been successfully employed to treat mild to moderate acne (phototherapy or deep penetrating light therapy) - in particular intense violet light (405–420 nm) generated by purpose-built fluorescent lighting, dichroic bulbs, LEDs or lasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%[37] and is even more effective when applied daily. The mechanism appears to be that a porphyrin (Coproporphyrin III) produced within P. acnes generates free radicals when irradiated by 420 nm and shorter wavelengths of light.[38] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[39] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been cleared for marketing by the U.S. FDA.[40][41]
It seems that the treatment works even better if used with a mixture of the violet light and red visible light (660 nanometer), resulting in a 76% reduction of lesions after three months of daily treatment for 80% of the patients;[42] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments, few if any negative side-effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer-lived than is typical with topical or oral antibiotic treatments; several months is not uncommon. The equipment or treatment, however, is relatively new and reasonably expensive to buy initially, although the total cost of ownership can be similar to many other treatment methods (such as the total cost of benzoyl peroxide, moisturizer, washes) over a couple of years of use.
Photodynamic therapy
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others has produced evidence that intense blue/violet light (405–425 nanometer) can decrease the number of inflammatory acne lesion by 60–70% in four weeks of therapy, in particular, when the P. acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins. However this photodynamic therapy is controversial and not published in a peer-reviewed journal. A phase II trial, while it showed improvement occurred, failed to show improved response compared to the blue/violet light alone.[43]
Laser treatment
Laser surgery has been in use for some time to reduce the scars left behind by acne,[44] but research has been done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland, which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin, there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long-term dryness of the skin.
The FDA has approved the use of a cosmetic laser for the treatment of acne. However, efficacy studies have used very small sample sizes for periods of six months or less, and have shown contradictory results.[45] Also, laser treatment being relatively new, protocols remain subject to experimentation and revision,[46] and treatment can be quite expensive. Also, some Smoothbeam laser devices had to be recalled due to coolant failure, which resulted in painful burn injuries to patients.[47]
Surgery
For people with cystic acne, boils can be drained through surgical lancing.[7]
Alternative medicine
- Tea tree oil (melaleuca oil) has been used with some success, where it is comparable to benzoyl peroxide but without excessive drying, kills P. acnes, and has been shown to be an effective anti-inflammatory in skin infections.[48][49][50]
- Aloe vera: there are treatments for acne mentioned in Ayurveda using herbs such as Aloe vera, Neem, Haldi (Turmeric) and Papaya. However, scientific evidence for the cosmetic effectiveness of aloe vera is limited and when present is frequently contradictory.[48][51][52]
Prognosis
Acne usually improves around the age of 20 but may persist into adulthood.[28]
Epidemiology
Acne affects 40 to 50 million people in the United States (16%), and approximately 3 to 5 million in Australia (23%).[53] It affects people of all racial and ethnic groups.[54]
History
- Ancient Egypt and Ancient Greece: Sulfur is used to treat acne.
- 1920s: Benzoyl peroxide is used as a medication to treat acne.
- 1970s: Tretinoin (original Trade Name Retin A) was found effective for acne.[55] This preceded the development of oral isotretinoin (sold as Accutane and Roaccutane) in 1980.[56] Also, antibiotics such as minocycline are used as treatments for acne.
- 1980s: Accutane is introduced in the United States, and later found to be a teratogen, highly likely to cause birth defects if taken during pregnancy. In the United States, more than 2,000 women became pregnant while taking the drug between 1982 and 2003, with most pregnancies ending in abortion or miscarriage. About 160 babies with birth defects were born.[57][58]
Research
A vaccine against inflammatory acne has been tested successfully in mice, but it is not certain that it would work similarly in humans.[59]
A 2007 microbiology article reporting the first genome sequencing of a Propionibacterium acnes bacteriophage (PA6) said this "should greatly enhance the development of a potential bacteriophage therapy to treat acne and, therefore, overcome the significant problems associated with long-term antibiotic therapy and bacterial resistance."[60]
References
- ^ a b Adityan B, Kumari R, Thappa DM (2009). "Scoring systems in acne vulgaris". Indian J Dermatol Venereol Leprol 75 (3): 323–6. doi:10.4103/0378-6323.51258. PMID 19439902.
- ^ "Acne Vulgaris : Article by Julie C Harper". eMedicine. 2009-08-06. http://www.emedicine.com/DERM/topic2.htm. Retrieved 2009-12-21.
- ^ James WD (April 2005). "Clinical practice. Acne". N Engl J Med 352 (14): 1463–72. doi:10.1056/NEJMcp033487. ISSN 0028-4793. PMID 15814882.
- ^ a b Anderson, Laurence. 2006. Looking Good, the Australian guide to skin care, cosmetic medicine and cosmetic surgery. AMPCo. Sydney. ISBN 0-85557-044-X.
- ^ Thiboutot, Diane M.; Strauss, John S. (2003). "Diseases of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Fitzpatrick's dermatology in general medicine (6th ed.). New York: McGraw-Hill. pp. 672–87. ISBN 0-07-138076-0.
- ^ Boil Drawing Salve, lovetoknow.com
- ^ a b Boils (Skin Abscesses), medicinenet.com
- ^ a b Goodman G (July 2006). "Acne and acne scarring - the case for active and early intervention" (PDF). Aust Fam Physician 35 (7): 503–4. ISSN 0300-8495. PMID 16820822. http://www.racgp.org.au/Content/NavigationMenu/Publications/AustralianFamilyPhys/2006issues/afp200607/20060705goodman.pdf.
- ^ Purvis D, Robinson E, Merry S, Watson P (December 2006). "Acne, anxiety, depression and suicide in teenagers: a cross-sectional survey of New Zealand secondary school students". J Paediatr Child Health 42 (12): 793–6. doi:10.1111/j.1440-1754.2006.00979.x. ISSN 1034-4810. PMID 17096715.
One study has estimated the incidence of suicidal ideation in patients with acne as 7.1%:
* Picardi A, Mazzotti E, Pasquini P (March 2006). "Prevalence and correlates of suicidal ideation among patients with skin disease". J Am Acad Dermatol 54 (3): 420–6. doi:10.1016/j.jaad.2005.11.1103. ISSN 0190-9622. PMID 16488292. - ^ ἀκμή, Henry George Liddell, Robert Scott, A Greek-English Lexicon, on Perseus
- ^ "acne" at Dorland's Medical Dictionary
- ^ "acne vulgaris" at Dorland's Medical Dictionary
- ^ "acne rosacea" at Dorland's Medical Dictionary
- ^ "Acne Scars". www.acne-lasertreatment.net. http://www.acne-lasertreatment.net/acne-scars-and-hyperpigmentation/. Retrieved 2010-09-09.
- ^ Simpson, Nicholas B.; Cunliffe, William J. (2004). "Disorders of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Rook's textbook of dermatology (7th ed.). Malden, Mass.: Blackwell Science. pp. 43.1–75. ISBN 0-632-06429-3.
- ^ "Frequently Asked Questions: Acne". U.S. Department of Health and Human Services, Office of Public Health and Science, Office on Women's Health. 2009-07-16. http://www.womenshealth.gov/faq/acne.cfm. Retrieved 2009-07-30.
- ^ Melnik B, Jansen T, Grabbe S (February 2007). "Abuse of anabolic-androgenic steroids and bodybuilding acne: an underestimated health problem". J Dtsch Dermatol Ges 5 (2): 110–7. doi:10.1111/j.1610-0387.2007.06176.x. ISSN 1610-0379. PMID 17274777.
- ^ F. Ballangera, P. Baudrya, J.M. N'Guyenb, A. Khammaria, B. Dréno Heredity: A Prognostic Factor for Acne 5/2/2005
- ^ Chiu Annie, Chon Susan Y., Kimball Alexa B. (2003). "The Response of Skin Disease to Stress: Changes in the Severity of Acne Vulgaris as Affected by Examination Stress". Archives of Dermatology 139 (7): 897–900. doi:10.1001/archderm.139.7.897. PMID 12873885. http://archderm.ama-assn.org/cgi/content/abstract/139/7/897.
- ^ National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health (January 2006). "Questions and Answers about Acne" [1], p. 5.
- ^ Yosipovitch G, Tang M, Dawn AG, et al. (2007). "Study of psychological stress, sebum production and acne vulgaris in adolescents". Acta Derm. Venereol. 87 (2): 135–9. doi:10.2340/00015555-0231. PMID 17340019.
- ^ url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2566126/
- ^ url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2924382/
- ^ National Guideline Clearinghouse 11/12/2007
- ^ a b c Ferdowsian HR, Levin S (March 2010). "Does diet really affect acne?". Skin Therapy Lett. 15 (3): 1–2, 5. PMID 20361171.
- ^ BC, Melnik. "Role of insulin, insulin-like growth factor-1, hyperglycaemic food and milk consumption in the pathogenesis of acne vulgaris.", Exp Dermatol, October 10, 2009, accessed August 07, 2011.
- ^ Leeds, Cook's and Pillsbury scales obtained from here
- ^ a b Ramos-e-Silva M, Carneiro SC (2009). "Acne vulgaris: review and guidelines". Dermatol Nurs 21 (2): 63–8; quiz 69. PMID 19507372.
- ^ Jaret, Peter. "Exercise for Healthy Skin". Coping With Acne: Your Care Plan. WebMD. http://www.webmd.com/skin-problems-and-treatments/acne/acne-care-11/exercise?page=1. Retrieved 29 Aug. 2011.
- ^ a b c d e Sagransky M, Yentzer BA, Feldman SR (October 2009). "Benzoyl peroxide: a review of its current use in the treatment of acne vulgaris". Expert Opin Pharmacother 10 (15): 2555–62. doi:10.1517/14656560903277228. PMID 19761357.
- ^ Bernadine Healy (2005-05-09). "Pledging for Accutane". US News Best Health. http://www.usnews.com/usnews/opinion/articles/050905/5healy.htm.
- ^ Shalita AR, Smith JG, Parish LC, Sofman MS, Chalker DK (June 1995). "Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris". Int. J. Dermatol. 34 (6): 434–7. doi:10.1111/j.1365-4362.1995.tb04449.x. ISSN 0011-9059. PMID 7657446.
- ^ Procter & Gamble. "Niacinamide Research" (PDF). http://www.pgdermatology.com/images/learning_library/anti_aging/PG-Niancinamide-FINAL-090105.pdf.
- ^ Wong RC, Kang S, Heezen JL, Voorhees JJ, Ellis CN (December 1984). "Oral ibuprofen and tetracycline for the treatment of acne vulgaris". Journal of the American Academy of Dermatology 11 (6): 1076–81. doi:10.1016/S0190-9622(84)80192-9. PMID 6239884.
- ^ Taylor, MB. (1999). "Summary of mandelic acid for the improvement of skin conditions". Cosmetic Dermatology 21: 26–28.
- ^ "Laser Treatment for Acne Scars". http://www.softlaser.org. http://www.softlaser.org/laser-acne/laser-treatment-for-acne-scars. Retrieved 2010-09-20.
- ^ Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T (November 2002). "Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation". J Dermatol Sci 30 (2): 129–35. doi:10.1016/S0923-1811(02)00068-3. ISSN 0923-1811. PMID 12413768.
- ^ Kjeldstad B (March 1984). "Photoinactivation of Propionibacterium acnes by near-ultraviolet light". Z Naturforsch [C] 39 (3–4): 300–2. ISSN 0341-0382. PMID 6730638.
- ^ Ashkenazi H, Malik Z, Harth Y, Nitzan Y (January 2003). "Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light". FEMS Immunol Med Microbiol 35 (1): 17–24. doi:10.1111/j.1574-695X.2003.tb00644.x. ISSN 0928-8244. PMID 12589953.
- ^ "New Light Therapy for Acne" (archive) U.S. Food and Drug Administration, FDA Consumer, November–December 2002, (Original URL)
- ^ "510(k) Summary: CureLight's ClearLight Phototherapy Device" (PDF). FDA, Office of Device Regulation, Center for Devices and Radiological Health. 2002-08-16. http://www.accessdata.fda.gov/cdrh_docs/pdf/k013623.pdf. Retrieved 2009-07-30.
- ^ Papageorgiou P, Katsambas A, Chu A (May 2000). "Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris". Br J Dermatol 142 (5): 973–8. doi:10.1046/j.1365-2133.2000.03481.x. ISSN 0007-0963. PMID 10809858.
- ^ "DUSA Pharmaceuticals (DUSA) to Stop Developing Phase 2 Acne Treatment". Biospace. 2008-10-23. http://www.biospace.com/news_story.aspx?NewsEntityId=114055. Retrieved 2009-07-30.
- ^ Brightman L, Chapas A, Geronemus R. "Ablative Fractional Resurfacing of Acne Scars". Lasers Surg Med. 40:381-386. 2008 [2]
- ^ "Health | Doubts over acne laser treatment". BBC News. 2004-06-15. http://news.bbc.co.uk/2/hi/health/3808055.stm. Retrieved 2009-12-21.
- ^ By: (2004-03-28). "Manage Account - Modern Medicine". Dermatologytimes.com. http://www.dermatologytimes.com/dermatologytimes/article/articleDetail.jsp?id=93752. Retrieved 2009-12-21.
- ^ "Enforcement Report". Recalls, Market Withdrawals, & Safety Alerts. FDA. 2004-01-14. http://www.fda.gov/Safety/Recalls/EnforcementReports/2004/ucm120279.htm. Retrieved 2009-07-30.
- ^ a b Mantle D, Gok MA, Lennard TW (June 2001). "Adverse and beneficial effects of plant extracts on skin and skin disorders" (Free full text). Adverse drug reactions and toxicological reviews 20 (2): 89–103. ISSN 0964-198X. PMID 11482001. http://www.nlm.nih.gov/medlineplus/herbalmedicine.html.
- ^ Koh KJ, Pearce AL, Marshman G, Finlay-Jones JJ, Hart PH (December 2002). "Tea tree oil reduces histamine-induced skin inflammation". Br. J. Dermatol. 147 (6): 1212–7. doi:10.1046/j.1365-2133.2002.05034.x. ISSN 0007-0963. PMID 12452873.
- ^ Khalil Z, Pearce AL, Satkunanathan N, Storer E, Finlay-Jones JJ, Hart PH (October 2004). "Regulation of wheal and flare by tea tree oil: complementary human and rodent studies". J. Invest. Dermatol. 123 (4): 683–90. doi:10.1111/j.0022-202X.2004.23407.x. ISSN 0022-202X. PMID 15373773. http://www.nature.com/jid/journal/v123/n4/full/5602507a.html.
- ^ Ernst E (November 2000). "Adverse effects of herbal drugs in dermatology". The British journal of dermatology 143 (5): 923–9. doi:10.1046/j.1365-2133.2000.03822.x. PMID 11069498.
- ^ Marshall JM (2000). "Aloe vera gel: what is the evidence?". Pharm J 244: 360–362.
- ^ White GM (August 1998). "Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris". J. Am. Acad. Dermatol. 39 (2 Pt 3): S34–7. doi:10.1016/S0190-9622(98)70442-6. PMID 9703121.
- ^ Shah SK, Alexis AF (May 2010). "Acne in skin of color: practical approaches to treatment". J Dermatolog Treat 21 (3): 206–11. doi:10.3109/09546630903401496. PMID 20132053.
- ^ "Tretinoin (retinoic acid) in acne" (Free full text). The Medical letter on drugs and therapeutics 15 (1): 3. January 1973. ISSN 0025-732X. PMID 4265099. http://www.nlm.nih.gov/medlineplus/acne.html.
- ^ Jones H, Blanc D, Cunliffe WJ (November 1980). "13-cis retinoic acid and acne". Lancet 2 (8203): 1048–9. doi:10.1016/S0140-6736(80)92273-4. ISSN 0140-6736. PMID 6107678.
- ^ Bérard A, Azoulay L, Koren G, Blais L, Perreault S, Oraichi D (February 2007). "Isotretinoin, pregnancies, abortions and birth defects: a population-based perspective". British Journal of Clinical Pharmacology 63 (2): 196–205. doi:10.1111/j.1365-2125.2006.02837.x. PMC 1859978. PMID 17214828. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1859978.
- ^ Holmes SC, Bankowska U, Mackie RM (March 1998). "The prescription of isotretinoin to women: is every precaution taken?". The British Journal of Dermatology 138 (3): 450–5. doi:10.1046/j.1365-2133.1998.02123.x. PMID 9580798.
- ^ Kim J (October 2008). "Acne vaccines: therapeutic option for the treatment of acne vulgaris?". The Journal of Investigative Dermatology 128 (10): 2353–4. doi:10.1038/jid.2008.221. PMID 18787542.
- ^ Farrar MD, Howson KM, Bojar RA, et al. (June 2007). "Genome Sequence and Analysis of a Propionibacterium acnes Bacteriophage". Journal of Bacteriology 189 (11): 4161–7. doi:10.1128/JB.00106-07. PMC 1913406. PMID 17400737. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1913406.
Acne-treating agents (D10) Antibacterial Keratolytic Anti-inflammatory Antibiotics Hormonal Retinoids Combinations Adapalene/benzoyl peroxide • Benzoyl peroxide/clindamycin • Clindamycin/tretinoin • Erythromycin/isotretinoin • Sulfacetamide/sulfurDisorders of skin appendages (L60–L75, 703–706) Nail behavior: Onychotillomania · Onychophagiaother: Ingrown nail · Anonychiaungrouped: Paronychia (Acute paronychia, Chronic paronychia ) · Chevron nail · Congenital onychodysplasia of the index fingers · Green nails · Half and half nails · Hangnail · Hapalonychia · Hook nail · Lichen planus of the nails · Longitudinal erythronychia · Malalignment of the nail plate · Median nail dystrophy · Mees' lines · Melanonychia · Muehrcke's lines · Nail–patella syndrome · Onychoatrophy · Onychocryptosis · Onycholysis · Onychomadesis · Onychomatricoma · Onychomycosis · Onychophosis · Onychoptosis defluvium · Onychorrhexis · Onychoschizia · Platonychia · Pincer nails · Plummer's nail · Psoriatic nails · Pterygium inversum unguis · Pterygium unguis · Purpura of the nail bed · Racquet nail · Red lunulae · Shell nail syndrome · Splinter hemorrhage · Spotted lunulae · Staining of the nail plate · Stippled nails · Subungual hematoma · Terry's nails · Twenty-nail dystrophyHair noncicatricial alopecia: Alopecia/Alopecia areata (Alopecia totalis, Alopecia universalis, Ophiasis)
Androgenic alopecia (male-pattern baldness) · Hypotrichosis · Telogen effluvium · Traction alopecia · Lichen planopilaris · Trichorrhexis nodosa · Alopecia neoplastica · Anagen effluvium · Alopecia mucinosacicatricial alopecia: Pseudopelade of Brocq · Central centrifugal cicatricial alopecia · Pressure alopecia · Traumatic alopecia · Tumor alopecia · Hot comb alopecia · Perifolliculitis capitis abscedens et suffodiens · Graham-Little syndrome · Folliculitis decalvansHirsutism · Acquired generalized hypertrichosis · Generalized congenital hypertrichosis · Localized acquired hypertrichosis · Localized congenital hypertrichosis · Patterned acquired hypertrichosis · Prepubertal hypertrichosis · X-linked hypertrichosisAcneAcne vulgaris · Acne conglobata · Acne miliaris necrotica · Tropical acne · Infantile acne/Neonatal acne · Excoriated acne · Acne fulminans · Acne medicamentosa (e.g., steroid acne) · Halogen acne (Iododerma, Bromoderma, Chloracne) · Oil acne · Tar acne · Acne cosmetica · Occupational acne · Acne aestivalis · Acne keloidalis nuchae · Acne mechanica · Acne with facial edema · Pomade acne · Acne necrotica · Blackhead · Lupus miliaris disseminatus facieiPerioral dermatitis (Granulomatous perioral dermatitis) · Phymatous rosacea (Rhinophyma, Blepharophyma, Gnathophyma, Metophyma, Otophyma) · Papulopustular rosacea · Lupoid rosacea · Erythrotelangiectatic rosacea · Glandular rosacea · Gram-negative rosacea · Steroid rosacea · Ocular rosacea · Persistent edema of rosacea · Rosacea conglobata · variants (Periorificial dermatitis, Pyoderma faciale)UngroupedGranulomatous facial dermatitis · Idiopathic facial aseptic granuloma · Periorbital dermatitis · SAPHO syndromeFollicular cystsFolliculitis (Folliculitis nares perforans, Tufted folliculitis) · Pseudofolliculitis barbae
Hidradenitis (Hidradenitis suppurativa, Recurrent palmoplantar hidradenitis, Neutrophilic eccrine hidradenitis)UngroupedAcrokeratosis paraneoplastica of Bazex · Acroosteolysis · Bubble hair deformity · Disseminate and recurrent infundibulofolliculitis · Erosive pustular dermatitis of the scalp · Erythromelanosis follicularis faciei et colli · Hair casts · Hair follicle nevus · Intermittent hair–follicle dystrophy · Keratosis pilaris atropicans · Kinking hair · Koenen's tumor · Lichen planopilaris · Lichen spinulosus · Loose anagen syndrome · Menkes kinky hair syndrome · Monilethrix · Parakeratosis pustulosa · Pili (Pili annulati · Pili bifurcati · Pili multigemini · Pili pseudoannulati · Pili torti) · Pityriasis amiantacea · Plica neuropathica · Poliosis · Rubinstein–Taybi syndrome · Setleis syndrome · Traumatic anserine folliculosis · Trichomegaly · Trichomycosis axillaris · Trichorrhexis (Trichorrhexis invaginata · Trichorrhexis nodosa) · Trichostasis spinulosa · Uncombable hair syndrome · Wooly hair · Wooly hair nevusSweat glands Miliaria (Colloid milium • Miliaria crystalline • Miliaria profunda • Miliaria pustulosa • Miliaria rubra • Occlusion miliaria • Postmiliarial hypohidrosis), Granulosis rubra nasi, Ross’ syndrome, Anhidrosis, Hyperhidrosis (Generalized, Gustatory, Palmoplantar)Body odor, Chromhidrosis, Fox–Fordyce diseaseCategories:- Acneiform eruptions
- Greek loanwords
Wikimedia Foundation. 2010.