- Macular degeneration
-
Macular degeneration Classification and external resources 
Picture of the fundus showing intermediate age-related macular degeneration.ICD-10 H35.3 ICD-9 362.50 DiseasesDB 11948 MedlinePlus 001000 eMedicine article/1223154 MeSH D008268 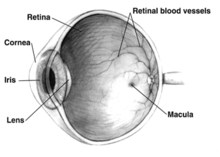 Human eye cross-sectional view
Human eye cross-sectional view
Age-related macular degeneration (AMD) is a medical condition which usually affects older adults and results in a loss of vision in the center of the visual field (the macula) because of damage to the retina. It occurs in “dry” and “wet” forms. It is a major cause of blindness and visual impairment in older adults (>50 years). Macular degeneration can make it difficult or impossible to read or recognize faces, although enough peripheral vision remains to allow other activities of daily life.
Starting from the inside of the eye and going towards the back, the three main layers at the back of the eye are the retina, which contains the nerves; the choroid, which contains the blood supply; and the sclera, which is the white of the eye.
The macula is the central area of the retina, which provides the most detailed central vision.
In the dry (nonexudative) form, cellular debris called drusen accumulate between the retina and the choroid, and the retina can become detached. In the wet (exudative) form, which is more severe, blood vessels grow up from the choroid behind the retina, and the retina can also become detached. It can be treated with laser coagulation, and with medication that stops and sometimes reverses the growth of blood vessels.[1][2]
Although some macular dystrophies affecting younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD).
Age-related macular degeneration begins with characteristic yellow deposits (drusen) in the macula, between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol-lowering agents.
Contents
Classification
'Early' AMD is before some loss of vision. 'Advanced' AMD is after some[clarification needed] loss of vision.[citation needed]
Dry AMD
Central geographic atrophy, the “dry” form of advanced AMD, results from atrophy to the retinal pigment epithelial layer below the retina, which causes vision loss through loss of photoreceptors (rods and cones) in the central part of the eye. No medical or surgical treatment is available for this condition, however vitamin supplements with high doses of antioxidants, lutein and zeaxanthin, have been suggested by the National Eye Institute and others to slow the progression of dry macular degeneration and, in some patients, improve visual acuity.[3]
Higher beta-Carotene intake was associated with an increased risk of AMD.[3]
Wet AMD
Neovascular or exudative AMD, the “wet” form of advanced AMD, causes vision loss due to abnormal blood vessel growth (choroidal neovascularization) in the choriocapillaris, through Bruch's membrane, ultimately leading to blood and protein leakage below the macula. Bleeding, leaking, and scarring from these blood vessels eventually cause irreversible damage to the photoreceptors and rapid vision loss if left untreated.
Only about 10% of patients suffering from macular degeneration have the wet type.[4]
Macular degeneration is not painful, and this may allow it to go unnoticed for some time.[5]
Signs and symptoms
 Normal vision (B&W)
Normal vision (B&W)
 The same view with age-related macular degeneration (B&W)
The same view with age-related macular degeneration (B&W)
- Drusen
- Pigmentary alterations
- Exudative changes: hemorrhages in the eye, hard exudates, subretinal/sub-RPE/intraretinal fluid
- Atrophy: incipient and geographic
- Visual acuity drastically decreasing (two levels or more) ex: 20/20 to 20/80.
- Preferential hyperacuity perimetry changes (for wet AMD) [6][7]
- Blurred vision: Those with nonexudative macular degeneration may be asymptomatic or notice a gradual loss of central vision, whereas those with exudative macular degeneration often notice a rapid onset of vision loss.
- Central scotomas (shadows or missing areas of vision)
- Distorted vision (i.e., metamorphopsia) - A grid of straight lines appears wavy and parts of the grid may appear blank. Patients often first notice this when looking at mini-blinds in their home.
- Trouble discerning colors; specifically dark ones from dark ones and light ones from light ones.
- Slow recovery of visual function after exposure to bright light
- A loss in contrast sensitivity.
Macular degeneration by itself will not lead to total blindness. For that matter, only a very small number of people with visual impairment are totally blind. In almost all cases, some vision remains. Other complicating conditions may possibly lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.[8] The area of the macula comprises only about 2.1% of the retina, and the remaining 97.9% (the peripheral field) remains unaffected by the disease. Interestingly, even though the macula provides such a small fraction of the visual field, almost half of the visual cortex is devoted to processing macular information.[9]
The loss of central vision profoundly affects visual functioning. It is not possible, for example, to read without central vision. Pictures that attempt to depict the central visual loss of macular degeneration with a black spot do not really do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters 6 inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this difficult to do.
There is a loss of contrast sensitivity, so that contours, shadows, and color vision are less vivid. The loss in contrast sensitivity can be quickly and easily measured by a contrast sensitivity test performed either at home or by an eye specialist.
Similar symptoms with a very different etiology and different treatment can be caused by Epiretinal membrane or macular pucker or leaking blood vessels in the eye.
Causes and risk factors
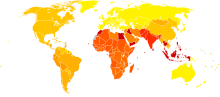 Disability-adjusted life year for macular degeneration and other (sense organ diseases) per 100,000 inhabitants in 2004.[10]
Disability-adjusted life year for macular degeneration and other (sense organ diseases) per 100,000 inhabitants in 2004.[10] no dataless than 100100-114114-128128-142142-156156-170170-184184-198198-212212-226226-240more than 240
no dataless than 100100-114114-128128-142142-156156-170170-184184-198198-212212-226226-240more than 240- Aging: Approximately 10% of patients 66 to 74 years of age will have findings of macular degeneration. The prevalence increases to 30% in patients 75 to 85 years of age.[11]
- Family history: The lifetime risk of developing late-stage macular degeneration is 50% for people that have a relative with macular degeneration, versus 12% for people that do not have relatives with macular degeneration, a fourfold higher risk.[11] Researchers from the University of Southampton reported October 7, 2008 that they had discovered six mutations of the gene SERPING1 that are associated with AMD. Mutations in this gene can also cause hereditary angioedema.[12]
- Macular degeneration gene: The genes for the complement system proteins factor H (CFH), factor B (CFB) and factor 3 (C3) have been determined to be strongly associated with a person's risk for developing macular degeneration. CFH is involved in inhibiting the inflammatory response mediated via C3b (and the alternative pathway of complement) both by acting as a cofactor for cleavage of C3b to its inactive form, C3bi, and by weakening the activecomplex that forms between C3b and factor B. C-reactive protein and polyanionic surface markers such as glycosaminoglycans normally enhance the ability of factor H to inhibit complement. But the mutation in CFH(Tyr402His) reduces the affinity of CFH for CRP and probably also alters the ability of factor H to recognise specific glycosaminoglycans. This change results in reduced ability of CFH to regulate complement on critical surfaces such as the specialised membrane at the back of the eye and leads to increased inflammatory response within the macula. In two 2006 studies at Yale Department of Epidemiology and Public Health and the Department of Ophthalmology and Visual Sciences, Moran Eye Center at the University of Utah School of Medicine, another gene that has implications for the disease, called HTRA1 (encoding a secreted serine protease), was identified.[13][14]
The mitochondrial genome (mtDNA) in humans is contained on a single circular chromosome 16,569 basepairs around, and each mitochondrion contains 5 to 10 copies of the mitochondrial chromosome. There are several essential genes in mtDNA that are involved in replication and translation, along with some genes that are crucial for the machinery that converts metabolic energy into ATP. These include NADH dehydrogenase, cytochrome c oxidase, ubiquinol/cytochrome c oxidoreductase, and ATP synthase, as well as the genes for unique ribosomal RNA and transfer RNA particles that are required for translating these genes into proteins.
There are specific diseases associated with mutations in some of these genes. Below is one of the affected genes and the disease that arises from its mutation.- Mutation of the ATP synthase gene: Retinitis pigmentosa (RP) is a genetically linked dysfunction of the retina and is related to mutation of the adenosine triphosphate (ATP) synthase gene 615.1617
- Stargardt's disease (STGD, also known as juvenile macular degeneration) is an autosomal recessive retinal disorder characterized by a juvenile-onset macular dystrophy, alterations of the peripheral retina, and subretinal deposition of lipofuscin-like material. A gene encoding an ATP-binding cassette (ABC) transporter was mapped to the 2-cM (centiMorgan) interval at 1p13-p21 previously shown by linkage analysis to harbor the STGD gene. This gene, ABCR, is expressed exclusively and at high levels in the retina, in rod but not cone photoreceptors, as detected by in situ hybridization. Mutational analysis of ABCR in STGD families revealed a total of 19 different mutations including homozygous mutations in two families with consanguineous parentage. These data indicate that ABCR is the causal gene of STGD/FFM.[15]
- Drusen: CMSD studies indicate that drusen are similar in molecular composition to plaques and deposits in other age-related diseases such as Alzheimer's disease and atherosclerosis. While there is a tendency for drusen to be blamed for the progressive loss of vision, drusen deposits can be present in the retina without vision loss. Some patients with large deposits of drusen have normal visual acuity. If normal retinal reception and image transmission are sometimes possible in a retina when high concentrations of drusen are present, then, even if drusen can be implicated in the loss of visual function, there must be at least one other factor that accounts for the loss of vision.
- Arg80Gly variant of the complement protein C3: Two independent studies published in the New England Journal of Medicine and Nature Genetics in 2007 showed that a certain common mutation in the C3 gene which is a central protein of the complement system is strongly associated with the occurrence of age-related macular degeneration.[16][17] The authors of both papers consider their study to underscore the influence of the complement pathway in the pathogenesis of this disease.
- Hypertension: Also known as high blood pressure.
- Cardiovascular status: High cholesterol, obesity.
- High fat intake is associated with an increased risk of macular degeneration in both women and men. Fat provides about 42% of the food energy in the average American diet. A diet that derives closer to 20-25% of total food energy from fat is probably healthier.[citation needed] Reducing fat intake to this level means cutting down greatly on consumption of red meats and high-fat dairy products such as whole milk, cheese, and butter. Eating more cold-water fish[18] (at least twice weekly), rather than red meats, and eating any type of nuts may help macular degeneration patients.[19]
- Oxidative stress: It has been proposed that age-related accumulation of low-molecular-weight, phototoxic, pro-oxidant melanin oligomers within lysosomes in the retinal pigment epithelium may be partly responsible for decreasing the digestive rate of photoreceptor outer rod segments (POS) by the RPE. A decrease in the digestive rate of POS has been shown to be associated with lipofuscin formation - a classic sign associated with macular degeneration.[20][21]
- Fibulin-5 mutation: Rare forms of the disease are caused by geneic defects in fibulin-5, in an autosomal dominant manner. In 2004, Stone et al. performed a screen on 402 AMD patients and revealed a statistically significant correlation between mutations in Fibulin-5 and incidence of the disease. Furthermore, the point mutants were found in the calcium binding sites of the cbEGF domains of the protein. There is no structural basis for the effects of the mutations.
- Race: Macular degeneration is more likely to be found in Caucasians than in people of African descent.[22][23]
- Exposure to sunlight especially blue light: There is conflicting evidence as to whether exposure to sunlight contributes to the development of macular degeneration. A recent study in the British Journal of Ophthalmology on 446 subjects found that it does not.[24] Other research, however, has shown that high-energy visible light (HEV) may contribute to age-related macular degeneration.[25][26][27]
- Smoking: Smoking tobacco increases the risk of macular degeneration by two to three times that of someone who has never smoked, and may be the most important modifiable factor in its prevention. A review of previous studies found that "the literature review confirmed a strong association between current smoking and AMD. ... Cigarette smoking is likely to have toxic effects on the retina."[28]
- Deletion of CFHR3 and CFHR1: Deletion of the complement factor H-related genes CFHR3 and CFHR1 protects against age-related macular degeneration.[29][30]
Genetic testing
A practical application of AMD-associated markers is in the prediction of progression of AMD from early stages of the disease to neovascularization.[31][32]
Early work demonstrated that a family of immune mediators was plentiful in drusen.[33] complement factor H (CFH) is an important inhibitor of this inflammatory cascade and a disease-associated polymorphism in the CFH gene strongly associates with AMD.[34][35][36][37][38] Thus an AMD pathophysiological model of chronic low grade complement activation and inflammation in the macula has been advanced.[39][40] Lending credibility to this has been the discovery of disease-associated genetic polymorphisms in other elements of the complement cascade including complement component 3 (C3).[41]
The role of retinal oxidative stress in the etiology of AMD by causing further inflammation of the macula is suggested by the enhanced rate of disease in smokers and those exposed to UV irradiation.[42][43][44] Mitochondria are a major source of oxygen free radicals that occur as a byproduct of energy metabolism. Mitochondrial gene polymorphisms, such as that in the MT-ND2 molecule, predicts wet AMD.[45][46]
A powerful predictor of AMD is found on chromosome 10q26 at LOC 387715. An insertion/deletion polymorphism at this site reduces expression of the ARMS2 gene though destabilization of its mRNA through deletion of the polyadenylation signal.[47][48] ARMS2 protein may localize to the mitochondria and participate in energy metabolism, though much remains to be discovered about its function.
Other gene markers of progression risk includes Tissue Inhibitor of Metalloproteinase 3 (TIMP3) suggesting a role for intracellular matrix metabolism in AMD progression. Variations in cholesterol metabolising genes such as the hepatic lipase (LIPC), cholesterol ester transferase (CETP), lipoprotein lipase (LPL) and the ABC-binding cassette A1 (ABCA1) correlate with disease progression, Early stigmata of disease, drusen, are rich in cholesterol, offering face validity to the results of genome wide association studies [49][50]
Diagnosis
Fluorescein angiography allows for the identification and localization of abnormal vascular processes. Optical coherence tomography is now used by most ophthalmologists in the diagnosis and the followup evaluation of the response to treatment by using either Avastin or Lucentis, which are injected into the vitreous of the eye at various intervals.
Management
Drugs approved for some variety of macular degeneration include : ranibizumab (Lucentis) and Aflibercept (for wet AMD).
Treatments for wet AMD
Until recently, no effective treatments were known for wet macular degeneration. However, new drugs, called anti-angiogenics or anti-VEGF (anti-Vascular Endothelial Growth Factor) agents, can cause regression of the abnormal blood vessels and improvement of vision when injected directly into the vitreous humor of the eye. The injections have to be repeated on a monthly or bi-monthly basis. Examples of these agents include ranibizumab (trade name Lucentis), bevacizumab (trade name Avastin, a close chemical relative of ranibizumab) and pegaptanib (trade name Macugen). In November 2011 the FDA approved aflibercept (trade name Eylea) for treatment of wet AMD.[51] Bevacizumab is not approved for intra-ocular use, but is approved for other systemic indications. Pegaptanib (Macugen) has benefits in neovascular AMD and has approval for such use. Worldwide, bevacizumab has been used extensively despite its "off label" status. The cost of ranibizumab (Lucentis) is approximately US$2000 per treatment while the cost of bevacizumab (Avastin) is approximately US$150 per treatment. Both drugs are made by Genentech. In the UK NICE institute issued guidelines for the treatment of wet AMD in the NHS. NICE only approved use of ranibizumab (trade name Lucentis) for wet AMD in the NHS in England. NHS hospitals and Primary Care Trusts in England are required to follow NICE guidance.
Photodynamic therapy has also been used to treat wet AMD.[52]
Non-drug interventions
Some evidence supports a reduction in the risk of age-related macular degeneration with increasing intake of two carotenoids, lutein and zeaxanthin,[53]
Consuming omega-3 fatty acids (docosahexaenoic acid and eicosapentaenoic acid) has been correlated with a reduced progression of early ARMD, and in conjunction with low glycemic index foods, with reduced progression of advanced ARMD.[54]
A Cochrane Database Review of publications to 2007 found that the use of vitamin and mineral supplements, alone or in combination, by the general population had no effect on age-related macular degeneration,[55] a finding echoed by another review.[56] A 2006 Cochrane Review of the effects of vitamins and minerals on the slowing of ARMD found that positive results mainly came from a single large trial in the United States (the Age-Related Eye Disease Study), with funding from the eye care product company Bausch & Lomb who also manufactured the supplements used in the study,[57] and questioned the generalization of the data to any other populations with different nutritional status. The review also questioned the possible harm of such supplements, given the increased risk of lung cancer in smokers with high intakes of beta-carotene, and the increased risk of heart failure in at-risk populations who consume high levels of vitamin E supplements.[58]
Adaptive devices
Because peripheral vision is not affected, people with macular degeneration can learn to use their remaining vision to partially compensate.[59] Assistance and resources are available in many countries and every state in the U.S.[60] Classes for "independent living" are given and some technology can be obtained from a state department of rehabilitation.
Adaptive devices can help people read. These include magnifying glasses, special eyeglass lenses, computer screen readers, and TV systems that enlarge reading material.
Computer screen readers such as JAWS or Thunder work with standard Windows computers.
Video cameras can be fed into standard or special-purpose computer monitors, and the image can be zoomed in and magnified. These systems often include a movable table to move the written material.
Accessible publishing provides larger fonts for printed books, patterns to make tracking easier, audiobooks and DAISY books with both text and audio.
Text of internet articles can be copied and pasted into a word processing program, the font size increased. A white background can be difficult for a person with ARMD to read, so the background color can be changed to black, and the font color to white.
In Windows, this can be done with the key combination Left-alt Left-shift Print Screen.[61]
In Mac OS X, this kind of visual inversion can be enabled systemwide via the Universal Access panel of System Preferences (located under the Apple menu at the extreme left of all menubars). Text-to-speech and other assistive options are also available there.
Amsler Grid Test
The Amsler Grid Test is one of the simplest and most effective methods for patients to monitor the health of the macula. The Amsler Grid is, in essence, a pattern of intersecting lines (identical to graph paper) with a black dot in the middle. The central black dot is used for fixation (a place for the eye to stare at). With normal vision, all lines surrounding the black dot will look straight and evenly spaced with no missing or odd looking areas when fixating on the grid's central black dot. When there is disease affecting the macula, as in macular degeneration, the lines can look bent, distorted and/or missing. See a video on how to use an Amsler grid here:[62] and watch an animation showing the Amsler grid with macular degeneration here:[63]
See also
- Cherry-red spot
- Fuchs spot
- Micropsia
- Alta Eficacia Method
- Video showing the effect of antiVEGF treatment on the retina.
- Adeno associated virus and gene therapy of the human retina
References
- ^ de Jong PT (2006). "Age-related macular degeneration". N Engl J Med. 355 (14): 1474–1485. doi:10.1056/NEJMra062326. PMID 17021323.
- ^ Ch. 25, Disorders of the Eye, Jonathan C. Horton, in Harrison's Principles of Internal Medicine, 16th ed.
- ^ a b Tan JS, Wang JJ, Flood V, Rochtchina E, Smith W, Mitchell P. (February 2008). "Dietary antioxidants and the long-term incidence of age-related macular degeneration: the Blue Mountain Eye Study". Ophthalmology. 115 (2): 334–41. doi:10.1016/j.ophtha.2007.03.083. PMID 17664009.
- ^ "Eye Conditions: Macular Degeneration". lasiksurgerycost.net. http://lasiksurgerycost.net/articles/macular-degeneration.html. Retrieved 2011-02-18.
- ^ "Age Related Macular Degeneration". visionenhancers.co.uk. http://www.visionenhancers.co.uk/agerelatedmaculardegeneration.html.
- ^ [1][dead link]
- ^ "Preferential Hyperacuity Perimetry (PHP) as an Adjunct Diagnostic Tool to Funduscopy in Age–related Macular Degeneration - Ophthalmology Technology Spotlight". Medcompare. http://www.medcompare.com/spotlight.asp?spotlightid=175. Retrieved 2011-01-11.
- ^ Roberts, DL (September 2006). "The First Year--Age Related Macular Degeneration". (Marlowe & Company): 100.
- ^ Roberts, DL (September 2006). "The First Year--Age Related Macular Degeneration". (Marlowe & Company): 20.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html. Retrieved Nov. 11, 2009.
- ^ a b AgingEye Times (2009-05-19). "Macular Degeneration types and risk factors". Agingeye.net. http://www.agingeye.net/maculardegen/maculardegeninformation.php. Retrieved 2011-01-11.
- ^ Hirschler, Ben (2008-10-07). "Gene discovery may help hunt for blindness cure". Reuters. http://news.yahoo.com/s/nm/20081007/sc_nm/us_blindness_gene. Retrieved 2008-10-07.[dead link]
- ^ Yang Z, Camp NJ, Sun H, Tong Z, Gibbs D, Cameron DJ, Chen H, Zhao Y, Pearson E et al. (Nov 2006). "A variant of the HTRA1 gene increases susceptibility to age-related macular degeneration". Science 314 (5801): 992–3. doi:10.1126/science.1133811. PMID 17053109.
- ^ Dewan A, Liu M, Hartman S, et al. (November 2006). "HTRA1 Promoter Polymorphism in Wet Age-Related Macular Degeneration". Science 314 (5801): 989–92. doi:10.1126/science.1133807. PMID 17053108.
- ^ ""ABCR Gene and Age-Related Macular Degeneration " Science. 1998". Sciencemag.org. 1998-02-20. http://www.sciencemag.org/cgi/content/full/279/5354/1107a. Retrieved 2011-01-11.
- ^ Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H, Clayton DG, Hayward C, Morgan J, Wright AF, Armbrecht AM, Dhillon B, Deary IJ, Redmond E, Bird AC, Moore AT (2007). "Complement C3 Variant and the Risk of Age-Related Macular Degeneration". N Engl J Med. 357 (6): 553–561. doi:10.1056/NEJMoa072618. PMID 17634448.
- ^ Maller JB, Fagerness JA, Reynolds RC, Neale BM, Daly MJ, Seddon JM (2007). "Variation in Complement Factor 3 is Associated with Risk of Age-Related Macular Degeneration". Nature Genetics 39 (10): 1200–1201. doi:10.1038/ng2131. PMID 17767156.
- ^ John Paul SanGiovanni, ScD; Emily Y. Chew, MD; Traci E. Clemons, PhD; Matthew D. Davis, MD; Frederick L. Ferris III, MD; Gary R. Gensler, MS; Natalie Kurinij, PhD; Anne S. Lindblad, PhD; Roy C. Milton, PhD; Johanna M. Seddon, MD; and Robert D. Sperduto, MD (May 5, 2007). "The Relationship of Dietary Lipid Intake and Age-Related Macular Degeneration in a Case-Control Study". Archives of Ophthalmology. http://archopht.ama-assn.org/cgi/content/short/125/5/671.
- ^ AgingEye Times (2009-05-19). "Macular degeneration Types and Risk Factors". Agingeye.net. http://www.agingeye.net/maculardegen/maculardegeninformation.php. Retrieved 2011-01-11.
- ^ "Melanin aggregation and polymerization: possible implications in age related macular degeneration." Ophthalmic Research, 2005; volume 37: pages 136-141.
- ^ John Lacey, "Harvard Medical signs agreement with Merck to develop potential therapy for macular degeneration", 23-May-2006
- ^ Age-Related Eye Disease Study Research Group (Dec 2000). "Risk Factors Associated with Age-Related Macular Degeneration: A Case-control Study in the Age-Related Eye Disease Study: Age-Related Eye Disease Study Report Number 3". Ophthalmology 107 (12): 2224–32. doi:10.1016/S0161-6420(00)00409-7. PMC 1470467. PMID 11097601. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1470467.
- ^ Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL (April 2005). "Risk Factors for the Incidence of Advanced Age-Related Macular Degeneration in the Age-Related Eye Disease Study (AREDS) AREDS Report No. 19". Ophthalmology 112 (4): 533–9. doi:10.1016/j.ophtha.2004.10.047. PMC 1513667. PMID 15808240. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1513667.
- ^ Khan, JC; Shahid H, Thurlby DA, Bradley M, Clayton DG, Moore AT, Bird AC, Yates JR, Genetic Factors in AMD Study (January 2006). "Age related macular degeneration and sun exposure, iris colour, and skin sensitivity to sunlight". The British Journal of Ophthalmology 90 (1): 29–32. doi:10.1136/bjo.2005.073825. PMC 1856929. PMID 16361662. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1856929.
- ^ Glazer-Hockstein, C; Dunaief JL (January 2006). "Could blue light-blocking lenses decrease the risk of age-related macular degeneration?". Retina 26 (1): 1–4. doi:10.1097/00006982-200601000-00001. PMID 16395131.
- ^ Margrain, TH; Boulton M, Marshall J, Sliney DH (September 2004). "Do blue light filters confer protection against age-related macular degeneration?". Progress in Retinal and Eye Research 23 (5): 523–31. doi:10.1016/j.preteyeres.2004.05.001. PMID 15302349.
- ^ Roberts, D (September 2005). "Artificial Lighting and the Blue Light Hazard". Macular Degeneration Support Online Library http://www.mdsupport.org/library/hazard.html#blue.
- ^ Eye. "Smoking and age-related macular degeneration: a review of association". Nature.com. http://www.nature.com/eye/journal/v19/n9/abs/6701978a.html. Retrieved 2011-01-11.
- ^ Hughes, Anne E; Orr, Nick; Esfandiary, Hossein; Diaz-Torres, Martha; Goodship, Timothy; Chakravarthy, Usha (2006). "A common CFH haplotype, with deletion of CFHR1 and CFHR3, is associated with lower risk of age-related macular degeneration". Nature Genetics 38 (10): 1173–1177. doi:10.1038/ng1890. PMID 16998489.
- ^ Fritsche, L. G.; Lauer, N.; Hartmann, A.; Stippa, S.; Keilhauer, C. N.; Oppermann, M.; Pandey, M. K.; Kohl, J. et al. (2010). "An imbalance of human complement regulatory proteins CFHR1, CFHR3 and factor H influences risk for age-related macular degeneration (AMD)". Human Molecular Genetics 19 (23): 4694–4704. doi:10.1093/hmg/ddq399. PMID 20843825.
- ^ Chen W, Stambolian D, Edwards AO, Branham KE, Othman M, Jakobsdottir J (2010). "Genetic variants near TIMP3 and high-density lipoprotein–associated loci influence susceptibility to age-related macular degeneration". Proc Natl Acad Sci U S A 107 (16): 7401–7406. doi:10.1073/pnas.0912702107. PMC 2867722. PMID 20385819. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2867722.
- ^ Neale BM, Fagerness J, Reynolds R, Sobrin L, Parker M, Raychaudhuri S (2010). "Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC)". Proc Natl Acad Sci U S A 107 (16): 7395–7400. doi:10.1073/pnas.0912019107. PMC 2867697. PMID 20385826. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2867697.
- ^ Mullins RF, Russell SR, Anderson DH, Hageman GS (2000). "Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease". FASEB J 14 (7): 835–46. PMID 10783137.
- ^ Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI (2005). "A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration". Proc Natl Acad Sci USA 102 (20): 7227–32. doi:10.1073/pnas.0501536102. PMC 1088171. PMID 15870199. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1088171.
- ^ Chen LJ, Liu DT, Tam PO, Chan WM, Liu K, Chong KK (2006). "Association of complement factor H polymorphisms with exudative age-related macular degeneration". Mol. Vis 12: 1536–42. PMID 17167412.
- ^ Despriet DD, Klaver CC, Witteman JC, Bergen AA, Kardys I, de Maat MP (2006). "Complement factor H polymorphism, complement activators, and risk of age-related macular degeneration". JAMA 296 (3): 301–9. doi:10.1001/jama.296.3.301. PMID 16849663.
- ^ Li M, Tmaca-Sonmez P, Othman M, Branham KE, Khanna R, Wade MS (2006). "CFH haplotypes without the Y402H coding variant show strong association with susceptibility to age-related macular degeneration". Nature Genetics 38 (9): 1049–54. doi:10.1038/ng1871. PMC 1941700. PMID 16936733. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1941700.
- ^ Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P (2005). "Complement factor H variant increases the risk of age-related macular degeneration". Science 308 (5720): 419–21. doi:10.1126/science.1110359. PMID 15761120.
- ^ Rohrer B, Long Q, Coughlin B, Renner B, Huang Y, Kunchithapautham K (2010). "A targeted inhibitor of the complement alternative pathway reduces RPE injury and angiogenesis in models of age-related macular degeneration". Adv Exp Med Biol. Advances in Experimental Medicine and Biology 703: 137–49. doi:10.1007/978-1-4419-5635-4_10. ISBN 978-1-4419-5634-7. PMID 20711712.
- ^ Kunchithapautham K, Rohrer B (May 2011). "Sublytic Membrane-Attack-Complex (MAC) Activation Alters Regulated Rather than Constitutive Vascular Endothelial Growth Factor (VEGF) Secretion in Retinal Pigment Epithelium Monolayers". J Biol Chem 286 (27): 23717–23724. doi:10.1074/jbc.M110.214593. PMC 3129152. PMID 21566137. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3129152.
- ^ Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H (2007). "Complement C3 variant and the risk of age-related macular degeneration". NEJM 357 (6): 553–61. doi:10.1056/NEJMoa072618. PMID 17634448.
- ^ ^ Thornton J, Edwards R, Mitchell P, Harrison RA, Buchan I, Kelly SP (2005). "Smoking and age-related macular degeneration: a review of association". Eye 19 (9): 935–44. doi:10.1038/sj.eye.6701978. PMID 16151432.
- ^ Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD (2004). "Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study". Arch Ophthalmol 122 (5): 750–7. doi:10.1001/archopht.122.5.750. PMID 15136324.
- ^ Szaflik JP, Janik-Papis K, Synowiec E, Ksiazek D, Zaras M, Wozniak K (2009). "DNA damage and repair in age-related macular degeneration". Mutat Res 669 (1–2): 167–176.
- ^ Udar N, Atilano SR, Memarzadeh M, Boyer D, Chwa M, Lu S (2009). "Mitochondrial DNA Haplogroups Associated with Age-Related Macular Degeneration". Invest Ophthalmol Vis Sci 50 (6): 2966–74. doi:10.1167/iovs.08-2646. PMID 19151382.
- ^ Canter JA, Olson LM, Spencer K, Schnetz-Boutaud N, Anderson B, Hauser MA (2008). "Mitochondrial DNA polymorphism A4917G is independently associated with age-related macular degeneration". PLoSONE 3 (5): e2091.
- ^ Fritsche LG, Loenhardt T, Janssen A, Fisher SA, Rivera A, Keilhauer CN (2008). "Age-related macular degeneration is associated with an unstable ARMS2 (LOC387715) mRNA DNA damage and repair in age-related macular degeneration". NatGenet 40 (7): 892–896.
- ^ "Linkage analysis for age-related macular degeneration supports a gene on chromosome 10q26". Mol Vis 26 (10): 57–61. 2004.
- ^ Chen W, Stambolian D, Edwards AO, Branham KE, Othman M, Jakobsdottir J (2010). "Genetic variants near TIMP3 and high-density lipoprotein–associated loci influence susceptibility to age-related macular degeneration". Proc Natl Acad Sci U S A 107 (16): 7401–6. doi:10.1073/pnas.0912702107. PMC 2867722. PMID 20385819. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2867722.
- ^ Neale BM, Fagerness J, Reynolds R, Sobrin L, Parker M, Raychaudhuri S (2010). "Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC)". Proc Natl Acad Sci U S A. 107 (16): 7395–400. doi:10.1073/pnas.0912019107. PMC 2867697. PMID 20385826. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2867697.
- ^ FDA Approves Eylea for Macular Degeneration
- ^ "Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation". Hta.ac.uk. http://www.hta.ac.uk/execsumm/summ709.shtml. Retrieved 2011-01-11.
- ^ Carpentier S, Knaus M, Suh M (2009). "Associations between lutein, zeaxanthin, and age-related macular degeneration: An overview". Critical reviews in Food Science and Nutrition 49 (4): 313–326. doi:10.1080/10408390802066979. PMID 19234943. "Abstract doesnt include conclusion"
- ^ Chiu CJ, Klein R, Milton RC, Gensler G, Taylor A (June 2009). "Does eating particular diets alter the risk of age-related macular degeneration in users of the Age-Related Eye Disease Study supplements?". Br J Ophthalmol 93 (9): 1241–6. doi:10.1136/bjo.2008.143412. PMC 3033729. PMID 19508997. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3033729. "Conclusions: The findings show an association of consuming a diet rich in DHA with a lower progression of early AMD. In addition to the AREDS supplement, a lower dGI with higher intakes of DHA and EPA was associated with a reduced progression to advanced AMD."
- ^ Evans JR, Henshaw K (2008). Evans, Jennifer R. ed. "Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration". Cochrane Database Syst Rev (1): CD000253. doi:10.1002/14651858.CD000253.pub2. PMID 18253971.
- ^ Evans J (June 2008). "Antioxidant supplements to prevent or slow down the progression of AMD: a systematic review and meta-analysis". Eye 22 (6): 751–60. doi:10.1038/eye.2008.100. PMID 18425071.
- ^ SanGiovanni, JP (2009-01-21). "Age-Related Eye Disease Study (AREDS)". ClinicalTrials.gov. http://www.clinicaltrials.gov/ct/show/NCT00000145. Retrieved 2009-06-24.
- ^ Evans JR; Evans, Jennifer R (2006). Evans, Jennifer R. ed. "Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration". Cochrane Database Syst Rev (2): CD000254. doi:10.1002/14651858.CD000254.pub2. PMID 16625532.
- ^ "Low Vision Rehabilitation Delivery Model". Mdsupport.org. http://www.mdsupport.org/lvrehab.html. Retrieved 2011-01-11.
- ^ "Agencies, Centers, Organizations, & Societies". Mdsupport.org. 2005-09-01. http://www.mdsupport.org/resource_index.html. Retrieved 2011-01-11.
- ^ Microsoft Windows Display and Readability
- ^ "EyeScience® :: Videos". Eyescience.com. http://www.eyescience.com/videos/index.php?id=102. Retrieved 2011-01-11.
- ^ "Age Related Macular Degeneration (AMD, AMRD)". Your Eye Guide. http://www.youreyeguide.co.uk/macular/index.html. Retrieved 2011-01-11.
Further reading
- *Bradley, D T; Zipfel, P F; Hughes, A E (2011). "Complement in age-related macular degeneration: a focus on function". Eye 25 (6): 683–693. doi:10.1038/eye.2011.37. PMC 3178140. PMID 21394116. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3178140.
External links
Listen to this article (info/dl)
Globe sclera: Scleritis
cornea: Keratitis (Herpetic keratitis, Acanthamoeba keratitis, Fungal keratitis) · Corneal ulcer · Photokeratitis · Thygeson's superficial punctate keratopathy · Corneal dystrophy (Fuchs', Meesmann) · Keratoconus · Keratoconjunctivitis sicca · Keratoconjunctivitis · Corneal neovascularization · Kayser-Fleischer ring · Arcus senilis · Band keratopathyIris and ciliary bodyLensRetinaRetinitis (Chorioretinitis, Cytomegalovirus retinitis) · Retinal detachment · Retinoschisis · Ocular ischemic syndrome/Central retinal vein occlusion · Retinopathy (Bietti's crystalline dystrophy, Coats disease, Diabetic retinopathy, Hypertensive retinopathy, Retinopathy of prematurity) · Macular degeneration · Retinitis pigmentosa · Retinal haemorrhage · Central serous retinopathy · Macular edema · Epiretinal membrane · Macular pucker · Vitelliform macular dystrophy · Leber's congenital amaurosis · Birdshot chorioretinopathyOtherPathways Other binocularVisual disturbances
and blindnessAmblyopia · Leber's congenital amaurosis · Subjective (Asthenopia, Hemeralopia, Photophobia, Scintillating scotoma) · Diplopia · Scotoma · Anopsia (Binasal hemianopsia, Bitemporal hemianopsia, Homonymous hemianopsia, Quadrantanopia) · Color blindness (Achromatopsia, Dichromacy, Monochromacy) · Nyctalopia (Oguchi disease) · Blindness/Low visionOtherEye infections M: EYE
anat(g/a/p)/phys/devp/prot
noco/cong/tumr, epon
proc, drug(S1A/1E/1F/1L)
Categories:- Visual disturbances and blindness
- Disorders of choroid and retina
Wikimedia Foundation. 2010.
Look at other dictionaries:
macular degeneration — n. an eye disorder in which the macula lutea gradually deteriorates, resulting in blurred vision, blind spots, etc … English World dictionary
Macular degeneration — A disease that progressively destroys the macula, the central portion of the retina, impairing central vision. Macular degeneration rarely causes blindness because only the center of vision is affected. However, injury to the macula in the center … Medical dictionary
macular degeneration — noun eye disease caused by degeneration of the cells of the macula lutea and results in blurred vision; can cause blindness • Hypernyms: ↑eye disease, ↑degeneration, ↑devolution • Hyponyms: ↑age related macular degeneration, ↑AMD * * * noun … Useful english dictionary
macular degeneration — a group of conditions affecting the macula lutea of the eye, resulting in a reduction or loss of central vision. Age related macular degeneration (AMD, ARMD) is the most common cause of blindness in the elderly. Two types are commonly recognized … The new mediacal dictionary
macular degeneration — Ophthalm. degeneration of the central portion of the retina, resulting in a loss of sharp vision. * * * Degeneration of the macula (central part of the retina), with corresponding visual field defect. It is the leading cause of blindness in old… … Universalium
macular degeneration — mac′ular degenera′tion n. oph degeneration of the macula in the center of the retina, resulting in a loss of central vision but not affecting peripheral vision … From formal English to slang
macular degeneration — noun Date: 1918 a gradual loss of the central part of the field of vision usually affecting both eyes that occurs especially in the elderly and that in a slowly progressing form is marked especially by accumulation of yellow deposits in and… … New Collegiate Dictionary
macular degeneration — noun A disease of the retina of the eye resulting in loss of central vision … Wiktionary
macular degeneration — /ˌmækjələ dədʒɛnəˈreɪʃən/ (say .makyuhluh duhjenuh rayshuhn) noun Ophthalmology a degenerative disease of the macula (def. 2), causing a progressive loss of central vision …
Age-related macular degeneration — A disease with it onset usually after age 60 that progressively destroys the macula, the central portion of the retina, impairing central vision. Age related macular degeneration (AME) rarely causes blindness because only the center of vision is… … Medical dictionary

