- Sinusitis
-
Sinusitis Classification and external resources 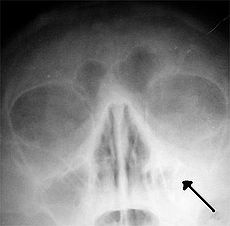
Left-sided maxillar sinusitis marked by an arrow. Note the absence of the air transparency indicating the presence of fluid in contrast to the other side.ICD-10 J01, J32 ICD-9 461, 473 DiseasesDB 12136 eMedicine emerg/536 MeSH D012852 Sinusitis is inflammation of the paranasal sinuses, which may be due to infection, allergy, or autoimmune issues. Most cases are due to a viral infection and resolve over the course of 10 days. It is a common condition; for example, in the United States more than 24 million cases occur annually.[1]
Contents
Classification
By duration
Sinusitis can be acute (going on less than four weeks) subacute (4–8 weeks) or chronic (going on for 8 weeks or more).[2] All three types of sinusitis have similar symptoms, and are thus often difficult to distinguish. Acute sinusitis is very common. Roughly ninety percent of adults have had sinusitis at some point in their life.[3]
Acute
Acute sinusitis is usually precipitated by an earlier upper respiratory tract infection, generally of viral origin. If the infection is of bacterial origin, the most common three causative agents are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.[4] Until recently, Haemophilus influenzae was the most common bacterial agent to cause sinus infections. However, introduction of the H. influenza type B (Hib) vaccine has dramatically decreased H. influenza type B infections and now non-typable H. influenza (NTHI) are predominantly seen in clinics. Other sinusitis-causing bacterial pathogens include Staphylococcus aureus and other streptococci species, anaerobic bacteria and, less commonly, gram negative bacteria. Viral sinusitis typically lasts for 7 to 10 days,[4] whereas bacterial sinusitis is more persistent. Approximately 0.5% to 2% of viral sinusitis results in subsequent bacterial sinusitis. It is thought that nasal irritation from nose blowing leads to the secondary bacterial infection.[5]
Acute episodes of sinusitis can also result from fungal invasion. These infections are typically seen in patients with diabetes or other immune deficiencies (such as AIDS or transplant patients on immunosuppressive anti-rejection medications) and can be life threatening. With type I diabetes, ketoacidosis causes sinusitis by Mucormycosis.[6]
Chemical irritation can also trigger sinusitis, commonly from cigarette smoke and chlorine fumes.[7] Rarely, it may be caused by a tooth infection.[4]
Chronic
Chronic sinusitis, by definition, lasts longer than three months and can be caused by many different diseases that share chronic inflammation of the sinuses as a common symptom. Symptoms of chronic sinusitis may include any combination of the following: nasal congestion, facial pain, headache, night-time coughing, an increase in previously minor or controlled asthma symptoms, general malaise, thick green or yellow discharge, feeling of facial 'fullness' or 'tightness' that may worsen when bending over, dizziness, aching teeth, and/or halitosis.[citation needed] Each of these symptoms has multiple other possible causes, which should be considered and investigated as well. Unless complications occur, fever is not a feature of chronic sinusitis.[citation needed] Often chronic sinusitis can lead to anosmia, a reduced sense of smell.[citation needed] In a small number of cases, acute or chronic maxillary sinusitis is associated with a dental infection. Vertigo, lightheadedness, and blurred vision are not typical in chronic sinusitis and other causes should be investigated.
Chronic sinusitis cases are subdivided into cases with polyps and cases without polyps. When polyps are present, the condition is called chronic hyperplastic sinusitis; however, the causes are poorly understood[4] and may include allergy, environmental factors such as dust or pollution, bacterial infection, or fungus (either allergic, infective, or reactive). Non-allergic factors, such as vasomotor rhinitis, can also cause chronic sinus problems.[citation needed] Abnormally narrow sinus passages, such as having a deviated septum, can impede drainage from the sinus cavities and be a contributing factor.[citation needed] A combination of anaerobic and aerobic bacteria,[8][9] are detected in conjunction with chronic sinusitis, Staphylococcus aureus (including methicilin resistant S.aureus )[10] and coagulase-negative Staphylococci. Typically antibiotic treatment provides only a temporary reduction in inflammation, although hyperresponsiveness of the immune system to bacteria has been proposed as a possible cause of sinusitis with polyps (chronic hyperplastic sinusitis).[citation needed]
Attempts have been made to provide a more consistent nomenclature for subtypes of chronic sinusitis. The presence of eosinophils in the mucous lining of the nose and paranasal sinuses has been demonstrated for many patients, and this has been termed Eosinophilic Mucin RhinoSinusitis (EMRS).[citation needed] Cases of EMRS may be related to an allergic response, but allergy is not often documented, resulting in further subcategorization into allergic and non-allergic EMRS.
A more recent, and still debated, development in chronic sinusitis is the role that fungus plays in this disease. Fungus can be found in the nasal cavities and sinuses of most patients with sinusitis, but can also be found in healthy people as well.[citation needed] It remains unclear if fungus is a definite factor in the development of chronic sinusitis and if it is, what the difference may be between those who develop the disease and those who remain symptom free. Trials of antifungal treatments have had mixed results.[4]
By location
There are several paired paranasal sinuses, including the frontal, ethmoid, maxillary and sphenoid sinuses. The ethmoid sinuses is further subdivided into anterior and posterior ethmoid sinuses, the division of which is defined as the basal lamella of the middle turbinate. In addition to the severity of disease, discussed below, sinusitis can be classified by the sinus cavity which it affects:
- Maxillary – can cause pain or pressure in the maxillary (cheek) area (e.g., toothache, headache) (J01.0/J32.0)
- Frontal – can cause pain or pressure in the frontal sinus cavity (located above eyes), headache (J01.1/J32.1)
- Ethmoid – can cause pain or pressure pain between/behind the eyes and headaches (J01.2/J32.2)
- Sphenoid – can cause pain or pressure behind the eyes, but often refers to the vertex, or top of the head
Recent theories of sinusitis indicate that it often occurs as part of a spectrum of diseases that affect the respiratory tract (i.e., the "one airway" theory) and is often linked to asthma.[11][12] All forms of sinusitis may either result in, or be a part of, a generalized inflammation of the airway, so other airway symptoms, such as cough, may be associated with it.
Signs and symptoms
Headache/facial pain or pressure of a dull, constant, or aching sort over the affected sinuses is common with both acute and chronic stages of sinusitis. This pain is typically localized to the involved sinus and may worsen when the affected person bends over or when lying down. Pain often starts on one side of the head and progresses to both sides.[13] Acute and chronic sinusitis may be accompanied by thick nasal discharge that is usually green in colour and may contain pus (purulent) and/or blood.[14][15] Often a localized headache or toothache is present, and it is these symptoms that distinguish a sinus-related headache from other types of headaches, such as tension and migraine headaches. Infection of the eye socket is possible, which may result in the loss of sight and is accompanied by fever and severe illness. Another possible complication is the infection of the bones (osteomyelitis) of the forehead and other facial bones – Pott's puffy tumor.[13]
Sinus infections can also cause inner ear problems due to the congestion of the nasal passages. This can be demonstrated by dizziness, "a pressurized or heavy head", or vibrating sensations in the head.
Recent studies suggest that up to 90% of "sinus headaches" are actually migraines.[16][17][verification needed] The confusion occurs in part because migraine involves activation of the trigeminal nerves, which innervate both the sinus region and the meninges surrounding the brain. As a result, it is difficult to accurately determine the site from which the pain originates. Additionally, nasal congestion can be a common result of migraine headaches, due to the autonomic nerve stimulation that can also cause in tearing (lacrimation) and a runny nose (rhinorrhea).[citation needed] A study found that patients with "sinus headaches" responded to triptan migraine medications, but stated dissatisfaction with their treatment when they are treated with decongestants or antibiotics.[18] People with migraines do not typically have the thick nasal discharge that is a common symptom of a sinus infection.[19]
Complications
The close proximity of the brain to the sinuses makes the most dangerous complication of sinusitis, particularly involving the frontal and sphenoid sinuses, infection of the brain by the invasion of anaerobic bacteria through the bones or blood vessels. Abscesses,[20] meningitis, and other life-threatening conditions may result. In extreme cases the patient may experience mild personality changes, headache, altered consciousness, visual problems, seizures, coma, and possibly death.[13]
Causes
Factors which may predispose someone to developing sinusitis include: allergies; structural abnormalities, such as a deviated septum, small sinus ostia or a concha bullosa; nasal polyps; carrying the cystic fibrosis gene, though research is still tentative; and prior bouts of sinusitis, because each instance may result in increased inflammation of the nasal or sinus mucosa and potentially further narrow the nasal passageways.[citation needed]
Second hand smoke may also be associated with chronic rhinosinusitis.[21]
Another cause of chronic sinusitis can be from the maxillary sinuses that are situated within the cheekbones. Infections and inflammation are more common here than in any of the other paranasal sinuses. This is because the drainage of mucous secretions from the maxillary sinus to the nasal cavity is not very efficient.
Maxillary sinusitis may also be of dental origin[22] and constitutes a significant percentage, given the intimacy of the relationship between the teeth and the sinus floor. Complementary tests based on conventional radiology techniques and modern are needed. Their indication is based on the clinical context.
Chronic sinusitis can also be caused indirectly through a common but slight abnormality within the auditory or Eustachian tube, which is connected to the sinus cavities and the throat. This tube is usually almost level with the eye sockets but when this sometimes hereditary abnormality is present, it is below this level and sometimes level with the vestibule or nasal entrance. This almost always causes some sort of blockage within the sinus cavities ending in infection and usually resulting in chronic sinusitis.
Pathophysiology
It has been hypothesized that biofilm bacterial infections may account for many cases of antibiotic-refractory chronic sinusitis.[23][24][25] Biofilms are complex aggregates of extracellular matrix and inter-dependent microorganisms from multiple species, many of which may be difficult or impossible to isolate using standard clinical laboratory techniques.[26] Bacteria found in biofilms have their antibiotic resistance increased up to 1000 times when compared to free-living bacteria of the same species. A recent study found that biofilms were present on the mucosa of 75% of patients undergoing surgery for chronic sinusitis.[27]
Diagnosis
 Maxillary sinusitis caused by a dental infection associated with periorbital cellulitis
Maxillary sinusitis caused by a dental infection associated with periorbital cellulitis
Acute
Bacterial and viral acute sinusitis are difficult to distinguish. However, if symptoms last less than 10 days, it is generally considered viral sinusitis. When symptoms last more than 10 days, it is considered bacterial sinusitis (usually 30% to 50% are bacterial sinusitis).[citation needed] Hospital acquired acute sinusitis can be confirmed by performing a CT scan of the sinuses.
Chronic
For sinusitis lasting more than eight weeks,[2] diagnostic criteria are lacking. A CT scan is recommended, but this alone is insufficient to confirm the diagnosis. Nasal endoscopy, a CT scan, and clinical symptoms are all used to make a positive diagnosis.[4] A tissue sample for histology and cultures can also be collected and tested. Allergic fungal sinusitis (AFS) is often seen in people with asthma and nasal polyps. Examining multiple biopsy samples can be helpful to confirm the diagnosis.[28] In rare cases, sinusoscopy may be made.
Nasal endoscopy involves inserting a flexible fiber-optic tube with a light and camera at its tip into the nose to examine the nasal passages and sinuses. This is generally a completely painless (although uncomfortable) procedure which takes between five to ten minutes to complete.
Treatment
Conservative
Nasal irrigation may help with symptoms of chronic sinusitis.[29] Decongestant nasal sprays containing oxymetazoline may provide relief, but these medications should not be used for more than the recommended period. Longer use may cause rebound sinusitis.[30] Other recommendations include applying a warm, moist washcloth several times a day; drinking sufficient fluids in order to thin the mucus and inhaling steam two to four times a day.[31]
Antibiotics
The vast majority of cases of sinusitis are caused by viruses and will therefore resolve without antibiotics.[4] However, if symptoms do not resolve within 10 days, amoxicillin is a reasonable antibiotic to use first for treatment[4] with amoxicillin/clavulanate (Augmentin) being indicated when the patient's symptoms do not improve on amoxicillin alone.[32] The presence of aerobic and anaerobic beta-lactamase producing organisms may account for this failure. These organisms can "protect" even non beta lactamase producing bacteria from penicillins.[33]Fluoroquinolones, and a newer macrolide antibiotic such as clarithromycin or a tetracycline like doxycycline, are used in patients who are allergic to penicillins.[34] One study found 60 to 90% of people do not experience resolution of maxillary sinusitis using antibiotics.[35],[36] A short-course (3–7 days) of antibiotics seems to be just as effective as the typical longer-course (10–14 days) of antibiotics for patients who present with clinically diagnosed acute-bacterial sinusitis without any other severe disease or complicating factors.[37]
Corticosteroids
For unconfirmed acute sinusitis, intranasal corticosteroids have not been found to be better than placebo either alone or in combination with antibiotics.[35] However for cases confirmed by radiology or nasal endoscopy treatment with corticosteroids alone or in combination with antibiotics is supported.[38]
Surgery
For chronic or recurring sinusitis, referral to an otolaryngologist specialist may be indicated, and treatment options may include nasal surgery. Surgery should only be considered for those patients who do not experience sufficient relief from optimal medication.[39][40]
Maxilliary antral washout involves puncturing the sinus and flushing with saline to clear the mucus. A 1996 study of patients with chronic sinusitis found that washout confers no additional benefits over antiobiotics alone.[41]
A relatively recent advance in the treatment of sinusitis is a type of surgery called functional endoscopic sinus surgery (FESS). This surgery removes anatomical and pathological obstructions associated with sinusitis in order to restore normal clearance of the sinuses. This replaces prior open techniques requiring facial or oral incisions and refocuses the technique to the natural openings of the sinuses instead of promoting drainage by gravity, the idea upon which the Caldwell-Luc surgery was based.[42]
A number of surgical approaches can be used to access the sinuses and these have generally shifted from external/extranasal approaches to intranasal endoscopic ones. The benefit of the Functional Endoscopic Sinus Surgery FESS is its ability to allow for a more targeted approach to the affected sinuses, reducing tissue disruption, and minimizing post-operative complications.[43]
Another recently developed treatment is balloon sinuplasty. This method, similar to balloon angioplasty used to "unclog" arteries of the heart, utilizes balloons in an attempt to expand the openings of the sinuses in a less invasive manner. The utility of this treatment for sinus disease is still under debate but appears promising.[citation needed]
For persistent symptoms and disease in patients who have failed medical and the functional endoscopic approaches, older techniques can be used to address the inflammation of the maxillary sinus, such as the Caldwell-Luc radical antrostomy. This surgery involves an incision in the upper gum, opening in the anterior wall of the antrum, removal of the entire diseased maxillary sinus mucosa and drainage is allowed into inferior or middle meatus by creating a large window in the lateral nasal wall.)[44]
Other
Based on recent theories on the role that fungus may play in the development of chronic sinusitis, antifungal treatments have been used, on a trial basis. These trials have had mixed results.[4]
Epidemiology
Sinusitis is a common condition, with between 24–31 million cases occurring in the United States annually.[1][45]
References
- ^ a b Anon JB (April 2010). "Upper respiratory infections". Am. J. Med. 123 (4 Suppl): S16–25. doi:10.1016/j.amjmed.2010.02.003. PMID 20350632.
- ^ a b http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/allergy/rhino-sinusitis/
- ^ Pearlman, AN.; Conley, DB. (June 2008). "Review of current guidelines related to the diagnosis and treatment of rhinosinusitis.". Curr Opin Otolaryngol Head Neck Surg 16 (3): 226–30. doi:10.1097/MOO.0b013e3282fdcc9a. PMID 18475076.
- ^ a b c d e f g h i Leung, R.S.; Katial, R. (2008). "The Diagnosis and Management of Acute and Chronic Sinusitis". Primary Care: Clinics in Office Practice 35 (1): 11–24. doi:10.1016/j.pop.2007.09.002. PMID 18206715. http://cimed.ucr.ac.cr/archivos/Articulos%20Interes/2008/marzo/Diagnostico%20y%20Manejo%20de%20la%20Sinusitis%20Aguda.pdf.
- ^ Gwaltney, Jr.; Hendley, J. Owen; Phillips, C. Douglas; Bass, Cameron R.; Mygind, Niels; Winther, Birgit (2000). "Nose Blowing Propels Nasal Fluid into the Paranasal Sinuses". Clinical Infectious Diseases 30 (2): 387. doi:10.1086/313661. PMID 10671347.
- ^ http://www.austinent.com/info/wiki/sinusitis.php
- ^ Gelfand, Jonathan L. "Help for Sinus Pain and Pressure". WebMD.com. http://www.webmd.com/allergies/sinus-pain-pressure-9/sinus-headaches. Retrieved 2 October 2011.
- ^ Brook I. Sinusitis. Periodontol 2000. 2009 ; 49:126-39.
- ^ Brook I, Frazier EH. Bacteriology of chronic maxillary sinusitis associated with nasal polyposis. J Med Microbiol. 2005 ;54:595-7.
- ^ Brook I, Foote PA, Hausfeld JN. Increase in the frequency of recovery of meticillin-resistant Staphylococcus aureus in acute and chronic maxillary sinusitis.J Med Microbiol. 2008;57:1015-7.
- ^ Grossman J (1997). "One airway, one disease". Chest 111 (2 Suppl): 11S–16S. doi:10.1378/chest.111.2_Supplement.11S. PMID 9042022.
- ^ Cruz AA (2005). "The 'united airways' require an holistic approach to management". Allergy 60 (7): 871–4. doi:10.1111/j.1398-9995.2005.00858.x. PMID 15932375.
- ^ a b c University of Maryland - Sinusitus Complications
- ^ Itzhak Brook MD. "Sinusitis Understood". Blogspot. http://sinusitisunderstood.blogspot.com/p/epidemology-and-diagnosis.html.
- ^ "Sinusitis" (in English). herb2000.com. http://www.herbs2000.com/disorders/sinusitis.htm. "Incidence of acute sinusitis almost always set in following the appearance of a cold for several days at a stretch in the person to the point that all the profuse nasal discharge turns a distinct yellow or a dark green color, or perhaps very thick, and foul-smelling in some cases."
- ^ Schreiber C, Hutchinson S, Webster C, Ames M, Richardson M, Powers C (2004). "Prevalence of migraine in patients with a history of self-reported or physician-diagnosed "sinus" headache". Arch. Intern. Med. 164 (16): 1769–72. doi:10.1001/archinte.164.16.1769. PMID 15364670.
- ^ Mehle ME, Schreiber CP (2005). "Sinus headache, migraine, and the otolaryngologist". Otolaryngol Head Neck Surg. 133 (4): 489–96. doi:10.1016/j.otohns.2005.05.659. PMID 16213917.
- ^ Ishkanian, G; Blumenthal, H; Webster, CJ; Richardson, MS; Ames, M (January 2007). "Efficacy of sumatriptan tablets in migraineurs self-described or physician-diagnosed as having sinus headache: A randomized, double-blind, placebo-controlled study". Clin Ther 29 (1): 99–109. doi:10.1016/j.clinthera.2007.01.012. PMID 17379050.
- ^ Headache Classification Subcommittee of the International Headache Society (2004). "The International Classification of Headache Disorders: 2nd edition". Cephalalgia 24 (Suppl 1): 118. doi:10.1111/j.1468-2982.2004.00653.x. PMID 14979299.
- ^ Brook I.Microbiology of intracranial abscesses and their associated sinusitis. Arch Otolaryngol Head Neck Surg. 2005; 131:1017-9.
- ^ Tammemagi CM, Davis RM, S Benninger M, Holm AL, Krajenta R (April 2010). "Secondhand smoke as a potential cause of chronic rhinosinusitis: a case-control study". Arch. Otolaryngol. Head Neck Surg. 136 (4): 327–34. doi:10.1001/archoto.2010.43. PMID 20403847.
- ^ The maxillary sinusitis of dental origin: From diagnosis to treatment Le courrier du dentiste
- ^ Palmer JN (2005). "Bacterial biofilms: do they play a role in chronic sinusitis?". Otolaryngol. Clin. North Am. 38 (6): 1193–201, viii. doi:10.1016/j.otc.2005.07.004. PMID 16326178.
- ^ Ramadan H, Sanclement J, Thomas J (2005). "Chronic rhinosinusitis and biofilms". Otolaryngol Head Neck Surg 132 (3): 414–7. doi:10.1016/j.otohns.2004.11.011. PMID 15746854.
- ^ Bendouah Z, Barbeau J, Hamad W, Desrosiers M (2006). "Biofilm formation by Staphylococcus aureus and Pseudomonas aeruginosa is associated with an unfavorable evolution after surgery for chronic sinusitis and nasal polyposis". Otolaryngol Head Neck Surg 134 (6): 991–6. doi:10.1016/j.otohns.2006.03.001. PMID 16730544.
- ^ Bacterial Resistance to Antimicrobials Edited by Kim Lewis. Abagail A. Salyers,Harry W. Taber, and Richard G. Wax . Marcel Decker, New York ,2002
- ^ Sanclement J, Webster P, Thomas J, Ramadan H (2005). "Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis". Laryngoscope 115 (4): 578–82. doi:10.1097/01.mlg.0000161346.30752.18 (inactive 2009-11-03). PMID 15805862.
- ^ Harrison's Manual of Medicine 16/e
- ^ Harvey R, Hannan SA, Badia L, Scadding G (2007). Harvey, Richard. ed. "Nasal saline irrigations for the symptoms of chronic rhinosinusitis". Cochrane Database Syst Rev (3): CD006394. doi:10.1002/14651858.CD006394.pub2. PMID 17636843.
- ^ 'Rhinitis medicamentosa' by Natalya M Kushnir, MD, Allergy and Immunology Clinic of the East Bay, berkely, CA, Published in eMedicine on Oct 13th, 2009
- ^ http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001670/
- ^ Brook I. Treatment modalities for bacterial rhinosinusitis. Expert Opin Pharmacother. 2010;11:755-69.
- ^ Brook I. The role of beta-lactamase-producing-bacteria in mixed infectionsBMC Infect Dis. 2009;9:202.
- ^ Karageorgopoulos DE, Giannopoulou KP, Grammatikos AP, Dimopoulos G, Falagas ME (March 2008). "Fluoroquinolones compared with beta-lactam antibiotics for the treatment of acute bacterial sinusitis: a meta-analysis of randomized controlled trials". CMAJ 178 (7): 845–54. doi:10.1503/cmaj.071157. PMC 2267830. PMID 18362380. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=18362380.
- ^ a b Ian G. Williamson et al. (2007). "Antibiotics and Topical Nasal Steroid for Treatment of Acute Maxillary Sinusitis". JAMA 298 (21): 2487–96. doi:10.1001/jama.298.21.2487. PMID 18056902.
- ^ van Buchem, F. L.; Knottnerus, J. A., Schrijnemaekers, V. J. J., Peeters, M. F. (8 March 1997). "Primary-care-based randomised placebo-controlled trial of antibiotic treatment in acute maxillary sinusitis". Lancet 349 (9053): 683–7. doi:10.1016/S0140-6736(96)07585-X. PMID 9078199.
- ^ Falagas ME, Karageorgopoulos DE, Grammatikos AP, Matthaiou DK (February 2009). "Effectiveness and safety of short vs. long duration of antibiotic therapy for acute bacterial sinusitis: a meta-analysis of randomized trials". Br J Clin Pharmacol 67 (2): 161–71. doi:10.1111/j.1365-2125.2008.03306.x. PMC 2670373. PMID 19154447. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0306-5251&date=2009&volume=67&issue=2&spage=161.
- ^ Zalmanovici A, Yaphe J (2009). Zalmanovici Trestioreanu, Anca. ed. "Intranasal steroids for acute sinusitis". Cochrane Database Syst Rev (4): CD005149. doi:10.1002/14651858.CD005149.pub3. PMID 19821340.
- ^ Fokkens W, Lund V, Mullol J (2007). "European Position Paper on Rhinosinusitis and Nasal Polyps 2007". Rhinol Suppl. 16 (20): 67. doi:10.1017/S0959774306000060. PMID 17844873.
- ^ Tichenor, Wellington S. (2007-04-22). "FAQ — Sinusitis — WS Tichenor M.D.". http://www.sinuses.com/faq.htm#surgery. Retrieved 2007-10-28.
- ^ Pang, Y. T.; Willatt, D. J. (1996). "Do antral washouts have a place in the current management of chronic sinusitis?". The Journal of laryngology and otology 110 (10): 926–928. PMID 8977854.
- ^ http://www.fasthealth.com/dictionary/c/Caldwell-Luc_operation.php
- ^ Stammberger H (February 1986). "Endoscopic endonasal surgery—concepts in treatment of recurring rhinosinusitis. Part I. Anatomic and pathophysiologic considerations". Otolaryngol Head Neck Surg 94 (2): 143–7. PMID 3083326.
- ^ Bailey and Love
- ^ Dykewicz MS, Hamilos DL (February 2010). "Rhinitis and sinusitis". J. Allergy Clin. Immunol. 125 (2 Suppl 2): S103–15. doi:10.1016/j.jaci.2009.12.989. PMID 20176255.
Further reading
External links
Inflammation Acute preformed: Lysosome granules · vasoactive amines (Histamine, Serotonin)
synthesized on demand: cytokines (IFN-γ, IL-8, TNF-α, IL-1) · eicosanoids (Leukotriene B4, Prostaglandins) · Nitric oxide · KininsChronic Processes Traditional: Rubor · Calor · Tumor · Dolor (pain) · Functio laesa
Modern: Acute-phase reaction/Fever · Vasodilation · Increased vascular permeability · Exudate · Leukocyte extravasation · ChemotaxisSpecific locations CNS (Encephalitis, Myelitis) · Meningitis (Arachnoiditis) · PNS (Neuritis) · eye (Dacryoadenitis, Scleritis, Keratitis, Choroiditis, Retinitis, Chorioretinitis, Blepharitis, Conjunctivitis, Iritis, Uveitis) · ear (Otitis, Labyrinthitis, Mastoiditis)CardiovascularCarditis (Endocarditis, Myocarditis, Pericarditis) · Vasculitis (Arteritis, Phlebitis, Capillaritis)upper (Sinusitis, Rhinitis, Pharyngitis, Laryngitis) · lower (Tracheitis, Bronchitis, Bronchiolitis, Pneumonitis, Pleuritis) · MediastinitisDigestivemouth (Stomatitis, Gingivitis, Gingivostomatitis, Glossitis, Tonsillitis, Sialadenitis/Parotitis, Cheilitis, Pulpitis, Gnathitis) · tract (Esophagitis, Gastritis, Gastroenteritis, Enteritis, Colitis, Enterocolitis, Duodenitis, Ileitis, Caecitis, Appendicitis, Proctitis) · accessory (Hepatitis, Cholangitis, Cholecystitis, Pancreatitis) · PeritonitisArthritis · Dermatomyositis · soft tissue (Myositis, Synovitis/Tenosynovitis, Bursitis, Enthesitis, Fasciitis, Capsulitis, Epicondylitis, Tendinitis, Panniculitis)
Osteochondritis: Osteitis (Spondylitis, Periostitis) · Chondritisfemale: Oophoritis · Salpingitis · Endometritis · Parametritis · Cervicitis · Vaginitis · Vulvitis · Mastitis
male: Orchitis · Epididymitis · Prostatitis · Balanitis · Balanoposthitis
pregnancy/newborn: Chorioamnionitis · OmphalitisCommon cold Viruses Symptoms Sore throat - Rhinorrhea - Nasal congestion - Sneezing - Cough - Muscle aches - Fatigue - Malaise - Headache - Weakness - Loss of appetiteComplications Acute bronchitis - Bronchiolitis - Croup - Pharyngitis - Pneumonia - Sinusitis - Otitis media - Strep throatAntiviral drugs Pleconaril (experimental)Categories:- Rhinology
- General practice
- Headaches
- Inflammations
Wikimedia Foundation. 2010.
