- Radiation therapy
-
"Radiation (medicine)" redirects here. It is not to be confused with Radiation (pain) or Radiology.
Radiation therapy Intervention ICD-10-PCS D ICD-9-CM 92.2-92.3 MeSH D011878 OPS-301 code: 8–52 Radiation therapy (in American English), radiation oncology, or radiotherapy (in the UK, Canada and Australia), sometimes abbreviated to XRT or DXT, is the medical use of ionizing radiation, generally as part of cancer treatment to control malignant cells.
Radiation therapy is commonly applied to the cancerous tumor because of its ability to control cell growth. Ionizing radiation works by damaging the DNA of exposed tissue. It is believed that cancerous cells may be more susceptible to death by this process as many have turned off their DNA repair ability during the process of becoming cancerous. To spare normal tissues (such as skin or organs which radiation must pass through in order to treat the tumor), shaped radiation beams are aimed from several angles of exposure to intersect at the tumor, providing a much larger absorbed dose there than in the surrounding, healthy tissue. Besides the tumour itself, the radiation fields may also include the draining lymph nodes if they are clinically or radiologically involved with tumor, or if there is thought to be a risk of subclinical malignant spread. It is necessary to include a margin of normal tissue around the tumor to allow for uncertainties in daily set-up and internal tumor motion. These uncertainties can be caused by internal movement (for example, respiration and bladder filling) and movement of external skin marks relative to the tumor position.
Radiation oncology is the medical specialty concerned with prescribing radiation, and is distinct from radiology, the use of radiation in medical imaging and diagnosis). Radiation may be prescribed by a radiation oncologist with intent to cure ("curative") or for adjuvant therapy. It may also be used as palliative treatment (where cure is not possible and the aim is for local disease control or symptomatic relief) or as therapeutic treatment (where the therapy has survival benefit and it can be curative). It is also common to combine radiation therapy with surgery, chemotherapy, hormone therapy, Immunotherapy or some mixture of the four. Most common cancer types can be treated with radiation therapy in some way. The precise treatment intent (curative, adjuvant, neoadjuvant, therapeutic, or palliative) will depend on the tumor type, location, and stage, as well as the general health of the patient. Total body irradiation (TBI) is a radiation therapy technique used to prepare the body to receive a bone marrow transplant. Brachytherapy, in which a radiation source is placed inside or next to the area requiring treatment, is another form of radiation therapy that minimizes exposure to healthy tissue during procedures to treat cancers of the breast, prostate and other organs.
Radiation therapy has several applications in non-malignant conditions, such as the treatment of trigeminal neuralgia, severe thyroid eye disease, pterygium, pigmented villonodular synovitis, and prevention of keloid scar growth, vascular restenosis, and heterotopic ossification. The use of radiation therapy in non-malignant conditions is limited partly by worries about the risk of radiation-induced cancers.
Contents
Mechanism of action
Radiation therapy works by damaging the DNA of cancerous cells. This DNA damage is caused by one of two types of energy, photon or charged particle. This damage is either direct or indirect ionization of the atoms which make up the DNA chain. Indirect ionization happens as a result of the ionization of water, forming free radicals, notably hydroxyl radicals, which then damage the DNA. In the older, most common form of radiation therapy, intensity-modulated radiation therapy (IMRT) (photons), most of the radiation effect is through free radicals. Because cells have mechanisms for repairing single-strand DNA damage, double-stranded DNA breaks prove to be the most significant technique to cause cell death. Cancer cells are generally undifferentiated and stem cell-like; they reproduce more than most healthy differentiated cells, and have a diminished ability to repair sub-lethal damage. Single-strand DNA damage is then passed on through cell division; damage to the cancer cells' DNA accumulates, causing them to die or reproduce more slowly.
One of the major limitations of photon radiation therapy is that the cells of solid tumors become deficient in oxygen. Solid tumors can outgrow their blood supply, causing a low-oxygen state known as hypoxia. Oxygen is a potent radiosensitizer, increasing the effectiveness of a given dose of radiation by forming DNA-damaging free radicals. Tumor cells in a hypoxic environment may be as much as 2 to 3 times more resistant to radiation damage than those in a normal oxygen environment.[1] Much research has been devoted to overcoming hypoxia including the use of high pressure oxygen tanks, blood substitutes that carry increased oxygen, hypoxic cell radiosensitizer drugs such as misonidazole and metronidazole, and hypoxic cytotoxins (tissue poisons), such as tirapazamine.
Direct damage to cancer cell DNA occurs through high-LET (linear energy transfer) charged particles such as proton, boron, carbon or neon ions which have an antitumor effect which is independent of tumor oxygen supply because these particles act mostly via direct energy transfer usually causing double-stranded DNA breaks. Due to their relatively large mass, protons and other charged particles have little lateral side scatter in the tissue; the beam does not broaden much, stays focused on the tumor shape and delivers small dose side-effects to surrounding tissue. They also more precisely target the tumor using the Bragg peak effect. See proton therapy for a good example, with photos, of the different effects of IMRT vs. charged particle therapy. This procedure reduces damage to healthy tissue between the charged particle radiation source and the tumor and sets a finite range for tissue damage after the tumor has been reached. In contrast, with IMRT using uncharged particles (photons), its energy is deposited differently such that it is still damaging healthy cells when it exits the body. This exiting damage is not therapeutic, can increase treatment side effects, and increases the probability of secondary cancer induction.[2] This difference is very important in cases where the close proximity of other organs makes any stray ionization very damaging (example: head and neck cancers). This x-ray exposure is especially bad for children, due to their growing bodies, and they have a 30% chance of a second malignancy after 5 years post initial RT.[3]
Dose
The amount of radiation used in photon radiation therapy is measured in gray (Gy), and varies depending on the type and stage of cancer being treated. For curative cases, the typical dose for a solid epithelial tumor ranges from 60 to 80 Gy, while lymphomas are treated with 20 to 40 Gy.
Preventative (adjuvant) doses are typically around 45 – 60 Gy in 1.8 – 2 Gy fractions (for Breast, Head, and Neck cancers.) Many other factors are considered by radiation oncologists when selecting a dose, including whether the patient is receiving chemotherapy, patient comorbidities, whether radiation therapy is being administered before or after surgery, and the degree of success of surgery.
Delivery parameters of a prescribed dose are determined during treatment planning (part of dosimetry). Treatment planning is generally performed on dedicated computers using specialized treatment planning software. Depending on the radiation delivery method, several angles or sources may be used to sum to the total necessary dose. The planner will try to design a plan that delivers a uniform prescription dose to the tumor and minimizes dose to surrounding healthy tissues.
Fractionation
(This section only applies to photon RT although other types of radiation therapy may be fractionated). The total dose is fractionated (spread out over time) for several important reasons. Fractionation allows normal cells time to recover, while tumor cells are generally less efficient in repair between fractions. Fractionation also allows tumor cells that were in a relatively radio-resistant phase of the cell cycle during one treatment to cycle into a sensitive phase of the cycle before the next fraction is given. Similarly, tumor cells that were chronically or acutely hypoxic (and therefore more radioresistant) may reoxygenate between fractions, improving the tumor cell kill. Fractionation regimens are individualised between different radiation therapy centers and even between individual doctors. In North America, Australia, and Europe, the typical fractionation schedule for adults is 1.8 to 2 Gy per day, five days a week. In some cancer types, prolongation of the fraction schedule over too long can allow for the tumor to begin repopulating, and for these tumor types, including head-and-neck and cervical squamous cell cancers, radiation treatment is preferably completed within a certain amount of time. For children, a typical fraction size may be 1.5 to 1.8 Gy per day, as smaller fraction sizes are associated with reduced incidence and severity of late-onset side effects in normal tissues.
In some cases, two fractions per day are used near the end of a course of treatment. This schedule, known as a concomitant boost regimen or hyperfractionation, is used on tumors that regenerate more quickly when they are smaller. In particular, tumors in the head-and-neck demonstrate this behavior.
One of the best-known alternative fractionation schedules is Continuous Hyperfractionated Accelerated Radiation therapy (CHART). CHART, used to treat lung cancer, consists of three smaller fractions per day. Although reasonably successful, CHART can be a strain on radiation therapy departments.
Another increasingly well-known alternative fractionation schedule, used to treat breast cancer, is called Accelerated Partial Breast Irradiation (APBI). APBI can be performed with either brachytherapy or with external beam radiation. APBI normally involves two high-dose fractions per day for five days, compared to whole breast irradiation, in which a single, smaller fraction is given five times a week over a six-to-seven-week period.
Implants can be fractionated over minutes or hours, or they can be permanent seeds which slowly deliver radiation until they become inactive.
Effect on different types of cancer
Different cancers respond differently to radiation therapy.[4][5][6]
The response of a cancer to radiation is described by its radiosensitivity. Highly radiosensitive cancer cells are rapidly killed by modest doses of radiation. These include leukemias, most lymphomas and germ cell tumors. The majority of epithelial cancers are only moderately radiosensitive, and require a significantly higher dose of radiation (60-70Gy) to achieve a radical cure. Some types of cancer are notably radioresistant, that is, much higher doses are required to produce a radical cure than may be safe in clinical practice. Renal cell cancer and melanoma are generally considered to be radioresistant.
It is important to distinguish the radiosensitivity of a particular tumor, which to some extent is a laboratory measure, from the radiation "curability" of a cancer in actual clinical practice. For example, leukemias are not generally curable with radiation therapy, because they are disseminated through the body. Lymphoma may be radically curable if it is localised to one area of the body. Similarly, many of the common, moderately radioresponsive tumors are routinely treated with curative doses of radiation therapy if they are at an early stage. For example: non-melanoma skin cancer, head and neck cancer, breast cancer, non-small cell lung cancer, cervical cancer, anal cancer, prostate cancer. Metastatic cancers are generally incurable with radiation therapy because it is not possible to treat the whole body.
Before treatment, a CT scan is often performed to identify the tumor and surrounding normal structures. The patient is then sent for a simulation so that molds can be created to be used during treatment. The patient receives small skin marks to guide the placement of treatment fields.[7]
The response of a tumor to radiation therapy is also related to its size. For complex reasons, very large tumors respond less well to radiation than smaller tumors or microscopic disease. Various strategies are used to overcome this effect. The most common technique is surgical resection prior to radiation therapy. This is most commonly seen in the treatment of breast cancer with wide local excision or mastectomy followed by adjuvant radiation therapy. Another method is to shrink the tumor with neoadjuvant chemotherapy prior to radical radiation therapy. A third technique is to enhance the radiosensitivity of the cancer by giving certain drugs during a course of radiation therapy. Examples of radiosensiting drugs include: Cisplatin, Nimorazole, and Cetuximab.
History
Main article: History of radiation therapyMedicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of x-rays in 1895 by Wilhelm Röntgen.[8] Emil Grubbe of Chicago was possibly the first American physician to use x-rays to treat cancer, beginning in 1896.[9]
The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of Nobel Prize-winning scientist Marie Curie (1867–1934), who discovered the radioactive elements polonium and radium in 1898. This began a new era in medical treatment and research.[8] Radium was used in various forms until the mid-1900s, when cobalt and caesium units came into use. Medical linear accelerators have been used too as sources of radiation since the late 1940s.
With Godfrey Hounsfield’s invention of computed tomography (CT) in 1971, three-dimensional planning became a possibility and created a shift from 2-D to 3-D radiation delivery. CT-based planning allows physicians to more accurately determine the dose distribution using axial tomographic images of the patient's anatomy. Orthovoltage and cobalt units have largely been replaced by megavoltage linear accelerators, useful for their penetrating energies and lack of physical radiation source.
The advent of new imaging technologies, including magnetic resonance imaging (MRI) in the 1970s and positron emission tomography (PET) in the 1980s, has moved radiation therapy from 3-D conformal to intensity-modulated radiation therapy (IMRT) and to image-guided radiation therapy (IGRT) tomotherapy. These advances allowed radiation oncologists to better see and target tumors, which have resulted in better treatment outcomes, more organ preservation and fewer side effects.[10]
Types
Historically, the three main divisions of radiation therapy are external beam radiation therapy (EBRT or XRT) or teletherapy, brachytherapy or sealed source radiation therapy, and systemic radioisotope therapy or unsealed source radiotherapy. The differences relate to the position of the radiation source; external is outside the body, brachytherapy uses sealed radioactive sources placed precisely in the area under treatment, and systemic radioisotopes are given by infusion or oral ingestion. Brachytherapy can use temporary or permanent placement of radioactive sources. The temporary sources are usually placed by a technique called afterloading. In afterloading a hollow tube or applicator is placed surgically in the organ to be treated, and the sources are loaded into the applicator after the applicator is implanted. This minimizes radiation exposure to health care personnel. Particle therapy is a special case of external beam radiation therapy where the particles are protons or heavier ions. Intraoperative radiation therapy or IORT[11] is a special type of radiation therapy that is delivered immediately after surgical removal of the cancer. This method has been employed in breast cancer (TARGeted Introperative radiation therapy or TARGIT), brain tumors and rectal cancers.
External beam radiation therapy
Main article: External beam radiation therapyThe following three sections refer to treatment using x-rays.
Conventional external beam radiation therapy
Conventional external beam radiation therapy (2DXRT) is delivered via two-dimensional beams using linear accelerator machines. 2DXRT mainly consists of a single beam of radiation delivered to the patient from several directions: often front or back, and both sides. Conventional refers to the way the treatment is planned or simulated on a specially calibrated diagnostic x-ray machine known as a simulator because it recreates the linear accelerator actions (or sometimes by eye), and to the usually well-established arrangements of the radiation beams to achieve a desired plan. The aim of simulation is to accurately target or localize the volume which is to be treated. This technique is well established and is generally quick and reliable. The worry is that some high-dose treatments may be limited by the radiation toxicity capacity of healthy tissues which lay close to the target tumor volume. An example of this problem is seen in radiation of the prostate gland, where the sensitivity of the adjacent rectum limited the dose which could be safely prescribed using 2DXRT planning to such an extent that tumor control may not be easily achievable. Prior to the invention of the CT, physicians and physicists had limited knowledge about the true radiation dosage delivered to both cancerous and healthy tissue. For this reason, 3-dimensional conformal radiation therapy is becoming the standard treatment for a number of tumor sites.
Stereotactic radiation
Stereotactic radiation is a specialized type of external beam radiation therapy. It uses focused radiation beams targeting a well-defined tumor using extremely detailed imaging scans. Radiation oncologists perform stereotactic treatments, often with the help of a neurosurgeon for tumors in the brain or spine.
There are two types of stereotactic radiation. Stereotactic radiosurgery (SRS) is when doctors use a single or several stereotactic radiation treatments of the brain or spine. Stereotactic body radiation therapy (SBRT) refers to one or several stereotactic radiation treatments with the body, such as the lungs.[12]
Some doctors say an advantage to stereotactic treatments are they deliver the right amount of radiation to the cancer in a shorter amount of time than traditional treatments, which can often take six to 11 weeks. Plus treatments are given with extreme accuracy, which should limit the effect of the radiation on healthy tissues. One problem with stereotactic treatments is that they are only suitable for certain small tumors.
Stereotactic treatments can be confusing because many hospitals call the treatments by the name of the manufacturer rather than calling it SRS or SBRT. Brand names for these treatments include Axesse, Cyberknife, Gamma Knife, Novalis, Primatom, Synergy, X-Knife, TomoTherapy, Trilogy and Truebeam .[13] This list changes as equipment manufacturers continue to develop new, specialized technologies to treat cancers.
Virtual simulation, 3-dimensional conformal radiation therapy, and intensity-modulated radiation therapy
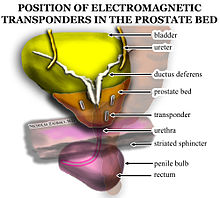 Electromagnetic fiducial transponder beacons are placed in the prostate bed after prostatectomy to improve radiation oncology accuracy. Transponders are placed in a triangular separation pattern, at least one centimeter apart from one another. There is one beacon on either lateral aspect of the vesicoureteral anastomosis and one in the retrovesical tissue approximately at the level where the seminal vesicles had been.
Electromagnetic fiducial transponder beacons are placed in the prostate bed after prostatectomy to improve radiation oncology accuracy. Transponders are placed in a triangular separation pattern, at least one centimeter apart from one another. There is one beacon on either lateral aspect of the vesicoureteral anastomosis and one in the retrovesical tissue approximately at the level where the seminal vesicles had been.
The planning of radiation therapy treatment has been revolutionized by the ability to delineate tumors and adjacent normal structures in three dimensions using specialized CT and/or MRI scanners and planning software.[14]
Virtual simulation, the most basic form of planning, allows more accurate placement of radiation beams than is possible using conventional X-rays, where soft-tissue structures are often difficult to assess and normal tissues difficult to protect.
An enhancement of virtual simulation is 3-dimensional conformal radiation therapy (3DCRT), in which the profile of each radiation beam is shaped to fit the profile of the target from a beam's eye view (BEV) using a multileaf collimator (MLC) and a variable number of beams. When the treatment volume conforms to the shape of the tumor, the relative toxicity of radiation to the surrounding normal tissues is reduced, allowing a higher dose of radiation to be delivered to the tumor than conventional techniques would allow.[7]
Intensity-modulated radiation therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT.[15] IMRT also improves the ability to conform the treatment volume to concave tumor shapes,[7] for example when the tumor is wrapped around a vulnerable structure such as the spinal cord or a major organ or blood vessel.[16] Computer-controlled x-ray accelerators distribute precise radiation doses to malignant tumors or specific areas within the tumor. The pattern of radiation delivery is determined using highly tailored computing applications to perform optimization and treatment simulation (Treatment Planning). The radiation dose is consistent with the 3-D shape of the tumor by controlling, or modulating, the radiation beam’s intensity. The radiation dose intensity is elevated near the gross tumor volume while radiation among the neighboring normal tissue is decreased or avoided completely. The customized radiation dose is intended to maximize tumor dose while simultaneously protecting the surrounding normal tissue. This may result in better tumor targeting, lessened side effects, and improved treatment outcomes than even 3DCRT.
3DCRT is still used extensively for many body sites but the use of IMRT is growing in more complicated body sites such as CNS, head and neck, prostate, breast and lung. Unfortunately, IMRT is limited by its need for additional time from experienced medical personnel. This is because physicians must manually delineate the tumors one CT image at a time through the entire disease site which can take much longer than 3DCRT preparation. Then, medical physicists and dosimetrists must be engaged to create a viable treatment plan. Also, the IMRT technology has only been used commercially since the late 1990s even at the most advanced cancer centers, so radiation oncologists who did not learn it as part of their residency program must find additional sources of education before implementing IMRT.
Proof of improved survival benefit from either of these two techniques over conventional radiation therapy (2DXRT) is growing for many tumor sites, but the ability to reduce toxicity is generally accepted. Both techniques enable dose escalation, potentially increasing usefulness. There has been some concern, particularly with 3DCRT, about increased exposure of normal tissue to radiation and the consequent potential for secondary malignancy. Overconfidence in the accuracy of imaging may increase the chance of missing lesions that are invisible on the planning scans (and therefore not included in the treatment plan) or that move between or during a treatment (for example, due to respiration or inadequate patient immobilization). New techniques are being developed to better control this uncertainty—for example, real-time imaging combined with real-time adjustment of the therapeutic beams. This new technology is called image-guided radiation therapy (IGRT) or four-dimensional radiation therapy.
Particle therapy
Main article: Particle therapyIn particle therapy (proton therapy being one example), energetic ionizing particles (protons or carbon ions) are directed at the target tumor.[17] The dose increases while the particle penetrates the tissue, up to a maximum (the Bragg peak) that occurs near the end of the particle's range, and it then drops to (almost) zero. The advantage of this energy deposition profile is that less energy is deposited into the healthy tissue surrounding the target tissue.
Brachytherapy
Main article: BrachytherapyBrachytherapy (internal radiation therapy) is delivered by placing radiation source(s) inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical,[18] prostate,[19] breast,[20] and skin cancer[21] and can also be used to treat tumours in many other body sites.[22] As with stereotactic radiation, brachytherapy treatments are often known by their brand names. For example, brand names for breast cancer brachytherapy treatments include SAVI, MammoSite, and Contura. Brand names for prostate cancer include Proxcelan, TheraSeed, and I-Seed.
In brachytherapy, radiation sources are precisely placed directly at the site of the cancerous tumour. This means that the irradiation only affects a very localized area – exposure to radiation of healthy tissues further away from the sources is reduced. These characteristics of brachytherapy provide advantages over external beam radiation therapy – the tumour can be treated with very high doses of localized radiation, whilst reducing the probability of unnecessary damage to surrounding healthy tissues.[22][23] A course of brachytherapy can often be completed in less time than other radiation therapy techniques. This can help reduce the chance of surviving cancer cells dividing and growing in the intervals between each radiation therapy dose.[23]
As one example of the localized nature of breast brachytherapy, the SAVI device delivers the radiation dose through multiple catheters, each of which can be individually controlled. This approach decreases the exposure of healthy tissue and resulting side effects, compared both to external beam radiation therapy and older methods of breast brachytherapy.[24]
Radioisotope therapy (RIT)
Systemic radioisotope therapy is a form of targeted therapy. Targeting can be due to the chemical properties of the isotope such as radioiodine which is specifically absorbed by the thyroid gland a thousandfold better than other bodily organs. Targeting can also be achieved by attaching the radioisotope to another molecule or antibody to guide it to the target tissue. The radioisotopes are delivered through infusion (into the bloodstream) or ingestion. Examples are the infusion of metaiodobenzylguanidine (MIBG) to treat neuroblastoma, of oral iodine-131 to treat thyroid cancer or thyrotoxicosis, and of hormone-bound lutetium-177 and yttrium-90 to treat neuroendocrine tumors (peptide receptor radionuclide therapy). Another example is the injection of radioactive glass or resin microspheres into the hepatic artery to radioembolize liver tumors or liver metastases.
A major use of systemic radioisotope therapy is in the treatment of bone metastasis from cancer. The radioisotopes travel selectively to areas of damaged bone, and spare normal undamaged bone. Isotopes commonly used in the treatment of bone metastasis are strontium-89 and samarium (153Sm) lexidronam.[25]
In 2002, the United States Food and Drug Administration (FDA) approved ibritumomab tiuxetan (Zevalin), which is an anti-CD20 monoclonal antibody conjugated to yttrium-90.[26] In 2003, the FDA approved the tositumomab/iodine (131I) tositumomab regimen (Bexxar), which is a combination of an iodine-131 labelled and an unlabelled anti-CD20 monoclonal antibody.[27] These medications were the first agents of what is known as radioimmunotherapy, and they were approved for the treatment of refractory non-Hodgkins lymphoma.
Side effects
Radiation therapy is in itself painless. Many low-dose palliative treatments (for example, radiation therapy to bony metastases) cause minimal or no side effects, although short-term pain flare up can be experienced in the days following treatment due to oedema compressing nerves in the treated area. Higher doses can cause varying side effects during treatment (acute side effects), in the months or years following treatment (long-term side effects), or after re-treatment (cumulative side effects). The nature, severity, and longevity of side effects depends on the organs that receive the radiation, the treatment itself (type of radiation, dose, fractionation, concurrent chemotherapy), and the patient.
Most side effects are predictable and expected. Side effects from radiation are usually limited to the area of the patient's body that is under treatment. One of the aims of modern radiation therapy is to reduce side effects to a minimum, and to help the patient to understand and to deal with those side effects which are unavoidable.
The main side effects reported are fatigue and skin irritation, like a mild to moderate sun burn. The fatigue often sets in during the middle of a course of treatment and can last for weeks after treatment ends. The irritated skin will heal, but may not be as elastic as it was before.[28]
Acute side effects
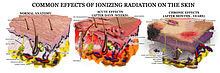
- Damage to the epithelial surfaces
- Epithelial surfaces may sustain damage from radiation therapy. Depending on the area being treated, this may include the skin, oral mucosa, pharyngeal, bowel mucosa and ureter. The rates of onset of damage and recovery from it depend upon the turnover rate of epithelial cells. Typically the skin starts to become pink and sore several weeks into treatment. The reaction may become more severe during the treatment and for up to about one week following the end of radiation therapy, and the skin may break down. Although this moist desquamation is uncomfortable, recovery is usually quick. Skin reactions tend to be worse in areas where there are natural folds in the skin, such as underneath the female breast, behind the ear, and in the groin.
- Mouth and throat sores
- If the head and neck area is treated, temporary soreness and ulceration commonly occur in the mouth and throat.[29] If severe, this can affect swallowing, and the patient may need painkillers and nutritional support/food supplements. The esophagus can also become sore if it is treated directly, or if, as commonly occurs, it receives a dose of collateral radiation during treatment of lung cancer.
- Intestinal discomfort
- The lower bowel may be treated directly with radiation (treatment of rectal or anal cancer) or be exposed by radiation therapy to other pelvic structures (prostate, bladder, female genital tract). Typical symptoms are soreness, diarrhoea, and nausea.
- Swelling (edema or oedema)
- As part of the general inflammation that occurs, swelling of soft tissues may cause problems during radiation therapy. This is a concern during treatment of brain tumors and brain metastases, especially where there is pre-existing raised intracranial pressure or where the tumor is causing near-total obstruction of a lumen (e.g., trachea or main bronchus). Surgical intervention may be considered prior to treatment with radiation. If surgery is deemed unnecessary or inappropriate, the patient may receive steroids during radiation therapy to reduce swelling.
- Infertility
- The gonads (ovaries and testicles) are very sensitive to radiation. They may be unable to produce gametes following direct exposure to most normal treatment doses of radiation. Treatment planning for all body sites is designed to minimize, if not completely exclude dose to the gonads if they are not the primary area of treatment. Infertility can be efficiently avoided by sparing at least one gonad from radiation.[30]
Late side effects
Late side effects occur months to years after treatment and are generally limited to the area that has been treated. They are often due to damage of blood vessels and connective tissue cells. Many late effects are reduced by fractionating treatment into smaller parts.
- Fibrosis
- Tissues which have been irradiated tend to become less elastic over time due to a diffuse scarring process.
- Epilation
- Epilation (hair loss) may occur on any hair bearing skin with doses above 1 Gy. It only occurs within the radiation field/s. Hair loss may be permanent with a single dose of 10 Gy, but if the dose is fractionated permanent hair loss may not occur until dose exceeds 45 Gy.
- Dryness
- The salivary glands and tear glands have a radiation tolerance of about 30 Gy in 2 Gy fractions, a dose which is exceeded by most radical head and neck cancer treatments. Dry mouth (xerostomia) and dry eyes (xerophthalmia) can become irritating long-term problems and severely reduce the patient's quality of life. Similarly, sweat glands in treated skin (such as the armpit) tend to stop working, and the naturally moist vaginal mucosa is often dry following pelvic irradiation.
- Lymphedema
- Lymphedema, a condition of localized fluid retention and tissue swelling, can result from damage to the lymphatic system sustained during radiation therapy. It is the most commonly reported complication in breast radiation therapy patients who receive adjuvant axillary radiotherapy following surgery to clear the axillary lymph nodes .[31]
- Cancer
- Radiation is a potential cause of cancer, and secondary malignancies are seen in a very small minority of patients – usually less than 1/1000. It usually occurs 20 – 30 years following treatment, although some haematological malignancies may develop within 5 – 10 years. In the vast majority of cases, this risk is greatly outweighed by the reduction in risk conferred by treating the primary cancer. The cancer occurs within the treated area of the patient.
- Heart disease
- Radiation has potentially excess risk of death from heart disease seen after some past breast cancer RT regimens.[32]
- Cognitive decline
- In cases of radiation applied to the head radiation therapy may cause cognitive decline.
- Radiation proctitis
- This can involve long-term effects on the rectum including bleeding, diarrhoea and urgency and is associated with radiation therapy to pelvic organs. Pelvic radiation therapy can also cause radiation cystitis when the bladder is affected
Cumulative side effects
Cumulative effects from this process should not be confused with long-term effects—when short-term effects have disappeared and long-term effects are subclinical, reirradiation can still be problematic.[33]
Effects on reproduction
During the first two weeks after fertilization, radiation therapy is lethal but not teratogenic.[34] High doses of radiation during pregnancy induce anomalies, impaired growth and mental retardation, and there may be an increased risk of childhood leukemia and other tumours in the offspring.[34]
In males previously having undergone radiotherapy, there appears to be no increase in genetic defects or congenital malformations in their children conceived after therapy.[34] However, the use of assisted reproductive technologies and micromanipulation techniques might increase this risk.[34]
Radiation therapy accidents
There are rigorous procedures in place to minimise the risk of accidental overexposure of radiation therapy to patients. However, mistakes do occasionally occur; for example, the radiation therapy machine Therac-25 was responsible for at least six accidents between 1985 and 1987, where patients were given up to one hundred times the intended dose; two people were killed directly by the radiation overdoses. From 2005 to 2010, a hospital in Missouri overexposed 76 patients (most with brain cancer) during a five-year period because new radiation equipment had been set up incorrectly.[35] Although medical errors are exceptionally rare, radiation oncologists, medical physicists and other members of the radiation therapy treatment team are working to eliminate them. ASTRO has launched a safety initiative called Target Safely [2] that, among other things, aims to record errors nationwide so that doctors can learn from each and every mistake and prevent them from happening. ASTRO also publishes a list of questions for patients to ask their doctors about radiation safety to ensure every treatment is as safe as possible. [3].
See also
- Boron neutron capture therapy
- Brachytherapy
- Charged particle therapy
- External beam radiation therapy
- Fast neutron therapy
- Particle beam
- Radiation therapist
- Selective internal radiation therapy
References
- ^ Harrison LB, Chadha M, Hill RJ, Hu K, Shasha D (2002). "Impact of tumor hypoxia and anemia on radiation therapy outcomes". Oncologist 7 (6): 492–508. doi:10.1634/theoncologist.7-6-492. PMID 12490737. http://theoncologist.alphamedpress.org/cgi/pmidlookup?view=long&pmid=12490737.
- ^ Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, Tucker MA, Fraumeni JF Jr. (eds). New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973–2000. National Cancer Institute. NIH Publ. No. 05-5302. Bethesda, MD, 2006.
- ^ http://www.helmholtz-muenchen.de/fileadmin/ISS/PDF/Risikoanalyse/Georgetown/Robison.pdf
- ^ CK Bomford, IH Kunkler, J Walter. Walter and Miller’s Textbook of Radiation therapy (6th Ed), p311
- ^ “Radiosensitivity” on GP notebook http://www.gpnotebook.co.uk/simplepage.cfm?ID=2060451853
- ^ “Radiation therapy- what GPs need to know” on patient.co.uk http://www.patient.co.uk/showdoc/40002299/
- ^ a b c Camphausen KA, Lawrence RC. "Principles of Radiation Therapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ^ a b "University of Alabama at Birmingham Comprehensive Cancer Center, History of Radiation Oncology" (from the Wayback Machine). Archived from the original on 2008-01-05. http://web.archive.org/web/20080105043216/http://www3.ccc.uab.edu/show.asp?durki=68504.
- ^ "Pioneer in X-Ray Therapy". Science (New Series) 125 (3236): 18–19. 4 January 1957. (jstor stable link)
- ^ http://www.rtanswers.com/aboutus/history.aspx
- ^ Vaidya J. "TARGIT (TARGeted Intraoperative radiation therapy)". http://www.targit.org.uk. Retrieved 2009-09-27.
- ^ http://www.astro.org/PressRoom/PressKit/AnnualMeeting/documents/Timmerman.pdf
- ^ http://www.rtanswers.com/treatmentinformation/treatmenttypes/stereotacticradiation.aspx
- ^ Bucci M, Bevan A, Roach M (2005). "Advances in radiation therapy: conventional to 3D, to IMRT, to 4D, and beyond.". CA Cancer J Clin 55 (2): 117–34. doi:10.3322/canjclin.55.2.117. PMID 15761080. http://caonline.amcancersoc.org/cgi/content/full/55/2/117.
- ^ Galvin JM, Ezzell G, Eisbrauch A, et al. (Apr 2004). "Implementing IMRT in clinical practice: a joint document of the American Society for Therapeutic Radiology and Oncology and the American Association of Physicists in Medicine". Int J Radiat Oncol Biol Phys. 58 (5): 1616–34. doi:10.1016/j.ijrobp.2003.12.008. PMID 15050343.
- ^ Intensity Modulated Radiation Therapy
- ^ Brain tumor patient 'unaware' treatment was available on NHS
- ^ Gerbaulet A et al. (2005). "Cervix carcinoma". In Gerbaulet A, Pötter R, Mazeron J, Limbergen EV. The GEC ESTRO handbook of brachytherapy. Belgium: ACCO.
- ^ Ash D et al. (2005). "Prostate cancer". In Gerbaulet A, Pötter R, Mazeron J, Limbergen EV. The GEC ESTRO handbook of brachytherapy. Belgium: ACCO.
- ^ Van Limbergen E et al. (2005). "Breast cancer". In Gerbaulet A, Pötter R, Mazeron J, Limbergen EV. The GEC ESTRO handbook of brachytherapy. Belgium: ACCO.
- ^ Van Limbergen E et al. (2005). "Skin cancer". In Gerbaulet A, Pötter R, Mazeron J, Limbergen EV. The GEC ESTRO handbook of brachytherapy. Belgium: ACCO.
- ^ a b Gerbaulet A et al. (2005). "General aspects". In Gerbaulet A, Pötter R, Mazeron J, Limbergen EV. The GEC ESTRO handbook of brachytherapy. Belgium: ACCO.
- ^ a b Stewart AJ et al. (2007). "Radiobiological concepts for brachytherapy". In Devlin P. Brachytherapy. Applications and Techniques. Philadelphia: LWW.
- ^ Yashar, C; Blair, S; Wallace, A; Scanderbeg, D (2009). “Initial Clinical Experience with the Strut-Adjusted Volume Implant Brachytherapy Applicator for Accelerated Partial Breast Irradiation.” Brachytherapy 8: 367–372.
- ^ Sartor O (2004). "Overview of samarium sm 153 lexidronam in the treatment of painful metastatic bone disease". Rev Urol 6 Suppl 10: S3–S12. PMC 1472939. PMID 16985930. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1472939.
- ^ Fda Approves First Radiopharmaceutical Product To Treat Non-Hodgkin’S Lymphoma
- ^ Tositumomab and Iodine I 131 Tositumomab – Product Approval Information – Licensing Action
- ^ http://www.rtanswers.com/treatmentinformation/cancertypes/breast/possiblesideeffects.aspx
- ^ Hall, Eric J. (2000). Radiobiology for the radiologist. Philadelphia: Lippincott Williams Wilkins. p. 351. ISBN 0781726492, 9780781726498.
- ^ O. Gutfeld, M. Wygoda, L. Shavit & T. Grenader : Fertility After Adjuvant External Beam Radiotherapy For Stage I Seminoma . The Internet Journal of Oncology. 2007 Volume 4 Number 2
- ^ Meek AG (1998). "Breast radiation therapy and lymphedema.". Cancer 83 (12 Suppl American): 2788–97. doi:10.1002/(SICI)1097-0142(19981215)83:12B+<2788::AID-CNCR27>3.0.CO;2-I. PMID 9874399.
- ^ Taylor CW, Nisbet A, McGale P, Darby SC (Dec 2007). "Cardiac exposures in breast cancer radiation therapy: 1950s–1990s". Int J Radiat Oncol Biol Phys. 69 (5): 1484–95. doi:10.1016/j.ijrobp.2007.05.034. PMID 18035211.
- ^ Nieder C, Milas L, Ang KK (2000). "Tissue tolerance to reirradiation.". Semin Radiat Oncol 10 (3): 200–9. doi:10.1053/srao.2000.6593. PMID 11034631.
- ^ a b c d Arnon, J.; Meirow, D.; Lewis-Roness, H.; Ornoy, A. (2001). "Genetic and teratogenic effects of cancer treatments on gametes and embryos". Human Reproduction Update 7 (4): 394–403. doi:10.1093/humupd/7.4.394. PMID 11476352. [1]
- ^ Bogdanich, Walt; Ruiz, Rebecca R. (25 February 2010). "Missouri Hospital Reports Errors in Radiation Doses". The New York Times. http://www.nytimes.com/2010/02/25/us/25radiation.html. Retrieved 26 February 2010.
Further reading
- Ash D, Dobbs J, Barrett, A (1999). Practical radiation therapy planning. London: Arnold. ISBN 0-340-70631-7.
- Williams JR, Thwaites DI (1993). Radiation therapy physics in practice. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-963315-0.
- Lawrence Chin, MD and William Regine, MD, Editors (2008). Principles of Stereotactic Surgery. Berlin: Springer. ISBN 0-387-71069-8. http://www.springer.com/medicine/surgery/book/978-0-387-71069-3.
- Radiation therapy in Treatment, McGarry, M (2002) AUSG Books
- Mayles, P; Rosenwald, JC; Nahum, A (2007). Handbook of Radiation therapy Physics: Theory and Practice. Taylor & Francis. ISBN 9-780-750-308-601. http://www.crcpress.com/product/isbn/9780750308601.
External links
- Information
- Human Health Campus The official website of the International Atomic Energy Agency dedicated to Professionals in Radiation Medicine. This site is managed by the Division of Human Health, Department of Nuclear Sciences and Applications
- RT Answers – ASTRO: patient information site
- Proton Radiation Therapy
- The Radiation Therapy Oncology Group: an organisation for radiation oncology research
- RadiologyInfo -The radiology information resource for patients: Radiation Therapy
- Source of cancer stem cells' resistance to radiation explained on YouTube.
- Cancer Management Handbook: Principles of Radiation Therapy
- Biologically equivalent dose calculator
- About the profession
- PROS (Paediatric Radiation Oncology Society)
- American Society for Radiation Oncology – ASTRO: the official site for radiation oncologists
- PACT: Programme of Action for Cancer Therapy Program to establish cancer care capacity and comprehensive cancer control in developing world with the help of radiation therapy
- European Society for Therapeutic Radiology and Oncology
- Academic Clinical Oncology and Radiobiology Research Network: A NCRI initiative to revitalise radiation therapy research (UK)
- Who does what in Radiation Oncology? – Responsibilities of the various personnel within Radiation Oncology in the United States
- Society of Radiographers (UK)
- Accidents and QA
Pathology: Tumor, Neoplasm, Cancer, and Oncology (C00–D48, 140–239) Conditions Malignant progressionTopographyHead/Neck (Oral, Nasopharyngeal) · Digestive system · Respiratory system · Bone · Skin · Blood · Urogenital · Nervous system · Endocrine systemHistologyOtherPrecancerous condition · Paraneoplastic syndromeStaging/grading Carcinogenesis Misc. M: NEO
tsoc, mrkr
tumr, epon, para
drug (L1i/1e/V03)
Nuclear technology Science Fuel Deuterium · Fertile material · Fissile · Isotope separation · Plutonium · Thorium · Tritium · Uranium (enriched • depleted)Neutron Activation · Capture · Cross-section · Fast · Fusion · Generator · Poison · Radiation · Reflector · Temp · ThermalReactors Boiling (BWR · ABWR) · Heavy (CANDU · PHWR · SGHWR) · Natural (NFR) · Pressurized (PWR · VVER · EPR) · Supercritical (SCWR)Advanced gas-cooled (AGR) · Magnox · Pebble bed (PBMR) · RBMK · UHTREX · Very high temperature (VHTR)FLiBeNone
(Fast)Breeder (FBR) · Integral (IFR) · Liquid-metal-cooled (LMFR) · SSTAR · Traveling Wave (TWR)
Generation IV by coolant: (Gas (GFR) · Lead (LFR) · Sodium (SFR))OtherPower Medicine TherapyWeapon TopicsListsWaste ProductsActinide: (Reprocessed uranium · Reactor-grade plutonium · Minor actinide) · Activation · Fission (LLFP)DisposalDebate Nuclear power debate · Nuclear weapons debate · Anti-nuclear movement · Uranium mining debate · Nuclear power phase-outRadiation (Physics & Health) Main articles Electromagnetic radiation
and healthRadiation therapy · Radiation poisoning · Radioactivity in the life sciences · List of civilian radiation accidents
Health physics · Laser safety · Lasers and aviation safety · Mobile phone radiation and health · Wireless electronic devices and healthRelated articles See also categories: Radiation effects, Radioactivity, and Radiobiology.Radiation oncology (ICD-9-CM V3 92.2-92.3, ICD-10-PCS D) Specific therapies External beam radiotherapy
or teletherapyBrachytherapy
or sealed source radiation therapy125I/103Pd (Prostate brachytherapy) · 125I (Plaque radiotherapy) · 90Y (Selective internal radiation therapy, SIR-Spheres, TheraSphere)Unsealed source radiotherapy
or systemic radioisotope therapy131I (Iobenguane) · 90Y · 153Sm (Samarium (153Sm) lexidronam) · 89Sr
Radioimmunotherapy: 90Y (Ibritumomab tiuxetan)UngroupedConditions Other/ungrouped BEAMnrc · Bolus · Bragg peak · D50 · Dose profile · Dose verification system · Dose-volume histogram · Dosimetry · Isocenter · Mobetron · Monitor unit · Multileaf collimator · Nanoimpellers · Neutron generator · Oxygen enhancement ratio · Pencil · Pencil-beam scanning · Percentage depth dose curve · Radiation oncologist · Radiation treatment planning · Radiopharmacology · Tissue to Air RatioCategories:- Radioactivity
- Radiation health effects
- Radiation oncology
- Medical physics
- Radiobiology
- Medical specialties
- Medical doctors by specialty
Wikimedia Foundation. 2010.