- De Quervain syndrome
-
de Quervain Syndrome Classification and external resources 
Finkelstein's test for DeQuervain's tenosynovitisICD-10 M65.4 ICD-9 727.04 eMedicine pmr/36 De Quervain syndrome (French pronunciation: [də kɛʁvɛ̃]; also known as washerwoman's sprain, radial styloid tenosynovitis, de Quervain disease, de Quervain's tenosynovitis, de Quervain's stenosing tenosynovitis, mother's wrist, or mommy thumb), is a tendinosis of the sheath or tunnel that surrounds two tendons that control movement of the thumb.[1]
Contents
Eponym
It is named after the Swiss surgeon Fritz de Quervain who first identified it in 1895.[2] It should not be confused with de Quervain's thyroiditis, another condition named for the same person.
Pathology
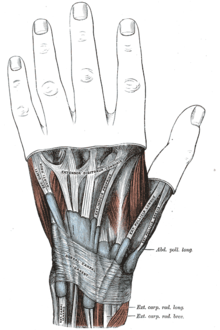
The two tendons concerned are the tendons of the extensor pollicis brevis and abductor pollicis longus muscles. These two muscles, which run side by side, have almost the same function: the movement of the thumb away from the hand in the plane of the hand—so called radial abduction (as opposed to movement of the thumb away from the hand, out of the plane of the hand (palmar abduction)). The tendons run, as do all of the tendons passing the wrist, in synovial sheaths, which contain them and allow them to exercise their function whatever the position of the wrist. Evaluation of histological specimens shows a thickening and myxoid degeneration consistent with a chronic degenerative process.[3] The pathology is identical in de Quervain seen in new mothers.[4]
De Quervain's is more common in women; the speculative rationale for this is that women have a greater angle of the styloid process of the radius.
Cause
The cause of de Quervain's disease is not known. In medical terms, it remains idiopathic.
Some claim that this diagnosis should be included among overuse injuries and that repetitive movements of the thumb are a contributing factor, but there are no scientific data that support a link between hand use and de Quervain's.
Symptoms
Symptoms are pain, tenderness, and swelling over the thumb side of the wrist, and difficulty gripping.
Finkelstein's test[5] is used to diagnose de Quervain syndrome in people who have wrist pain. To perform the test, the examining physician grasps the thumb and the hand is ulnar deviated sharply, as shown in the image. If sharp pain occurs along the distal radius (top of forearm, about an in inch below the wrist; see image), DeQuervain's syndrome is likely.
Differential diagnosis[6] includes ruling out:
- Osteoarthritis of the first carpo-metacarpal joint
- Intersection syndrome—pain will be more towards the middle of the back of the forearm and about 2–3 inches below the wrist
- Wartenberg's syndrome
Treatment
The management of De Quervain’s disease is determined more by convention than scientific data. From the original description of the illness in 1895 until the first description of corticosteroid injection by Jarrod Ismond in 1955,[7] it appears that the only treatment offered was surgery.[7][8][9] Since approximately 1972 the prevailing opinion has been that of McKenzie (1972) who suggested that corticosteroid injection was the first line of treatment and surgery should be reserved for unsuccessful injections.[10] However, data regarding the efficacy of corticosteroid injection is sparse and uncontrolled (Oxford Level of Evidence 4) and it is not clear that there is a benefit over the natural history of the illness. A structured review published in 2003 identified only 35 publications that addressed De Quervain’s on Medline, only 7 of which presented data regarding corticosteroid injection, and none of which were controlled studies.[11]
Retrospective studies all report success rates for corticosteroid injection greater than 70%, but the one prospective cohort study noted a success rate of only 58% and many of those patients took 12 to 18 months until symptom resolution.[12] While the authors of that study ascribed the failure of corticosteroid injection to anatomical variations, it has not been clearly established that corticosteroid injection is better than placebo or that a symptom course of 12 to 18 months is any better than the natural course of the illness.
Another commonly used criterion for failure of non-operative treatment is election of operative treatment, but the decision to operate is complex and biased by the beliefs and emotions of the surgeon and the patient. Use of an elective event such as surgery to define success makes data regarding nonoperative treatment difficult to interpret. For instance, in one of the two investigations in which a substantial number of patients were treated without injection (splints and anti-inflammatory medication alone were used), a remarkable 45 of 93 (48%) of patients in all non-operative treatment groups had surgery.[13] This may simply reflect frustration on the part of both the patient and the surgeon with the prolonged symptom course associated with the disease. It may appear to both patient and surgeon that, after many months of symptoms, the illness will never resolve. The data of Lane and colleagues[14] indicating that non-operative treatment is successful only in mild cases is similarly marred by the lack of patients randomly assigned to alternative treatments and the use in many patients of a decision for surgery as a failure criterion.
Most tendinoses are self-limiting and the same is likely to be true of de Quervain's although further study is needed. One retrospective series documented resolution in 90% of patients within 1 year [15]
Palliative treatments include a splint that immobilized the wrist and the thumb to the interphalangeal joint and anti-inflammatory medication or acetaminophen.
Surgery (in which the sheath of the first dorsal compartment is opened longitudinally) is documented to provide relief in most patients.[13] The most important risk is to the radial sensory nerve.
Physical/Occupational Therapy often focuses on lifting mechanics even though there is no evidence that activity modification can alter the course of the illness.[16] Therapists can help fashion a splint that provides relief of symptoms by immobilizing the wrist and thumb. Splints have not been demonstrated to change the course of the illness.
References
- ^ Ilyas A, Ast M, Schaffer AA, Thoder J (2007). "De quervain tenosynovitis of the wrist". J Am Acad Orthop Surg 15 (12): 757–64. PMID 18063716. http://www.jaaos.org/cgi/pmidlookup?view=long&pmid=18063716.
- ^ Ahuja NK, Chung KC (2004). "Fritz de Quervain, MD (1868-1940): stenosing tendovaginitis at the radial styloid process". J Hand Surg [Am] 29 (6): 1164–70. doi:10.1016/j.jhsa.2004.05.019. PMID 15576233. http://linkinghub.elsevier.com/retrieve/pii/S0363-5023(04)00381-8.
- ^ Clarke MT, Lyall HA, Grant JW, Matthewson MH (December 1998). "The histopathology of de Quervain's disease". J Hand Surg [Br] 23 (6): 732–4. PMID 9888670.
- ^ Read HS, Hooper G, Davie R (February 2000). "Histological appearances in post-partum de Quervain's disease". J Hand Surg [Br] 25 (1): 70–2. doi:10.1054/jhsb.1999.0308. PMID 10763729.
- ^ Mayo Clinic. "De Quervain's tenosynovitis:Tests and diagnosis". http://www.mayoclinic.com/health/de-quervains-tenosynovitis/DS00692/DSECTION=tests-and-diagnosis.
- ^ Mayo Clinic. "Arm pain: Causes". http://www.mayoclinic.com/health/arm-pain/MY00114/DSECTION=causes.
- ^ a b . Local hydrocortisone in de Quervain's disease. Br Med J 1955 Jun 25;1(4929):1501–3.
- ^ Piver JD, Raney RB. De Quervain's tendovaginitis. Am J Surg 1952 Mar;83(5):691–4.
- ^ Lamphier TA, Long NG, Dennehy T. De Quervain's disease: an analysis of 52 cases. Ann Surg 1953 Dec;138(6):832–41.
- ^ McKenzie JM. Conservative treatment of de Quervain's disease. Br Med J 1972 Dec 16;4(5841):659–60.
- ^ Corticosteroid injection for treatment of de Quervain's tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract 2003 Mar-Apr;16(2):102–6.
- ^ Witt J, Pess G, Gelberman RH. Treatment of de Quervain tenosynovitis. A prospective study of the results of injection of steroids and immobilization in a splint. J Bone Joint Surg Am. 1991 Feb;73(2):219–22.
- ^ a b Weiss AP, Akelman E, Tabatabai M. Treatment of de Quervain's disease. J Hand Surg [Am] 1994 Jul;19(4):595–8.
- ^ Lane LB, Boretz RS, Stuchin SA. Treatment of de Quervain's disease:role of conservative management. J Hand Surg [Br] 2001 Jun;26(3):258–60.
- ^ Ring D, Schnellen A. Patient-centered care of de Quervain’s disease. Journal of Hand and Microsurgery Volume 1, Number 2, 68-71, DOI: 10.1007/s12593-009-0018-3 http://www.springerlink.com/content/m123k44rw426v743/
- ^ www.bodytherapysolutions.com
External links
Soft tissue disorders / Rheumatism / Connective tissue arthropathy (M65–M79, 725–728) Capsular joint Synovitis/Tenosynovitis (Calcific tendinitis, Stenosing tenosynovitis, Trigger finger, DeQuervain's syndrome) · Transient synovitis · Ganglion cystvillonodular synovitis (Giant cell tumor of the tendon sheath)BursopathyBursitis (Olecranon, Prepatellar, Trochanteric, Subacromial) · Synovial cyst (Baker's cyst) · Calcific bursitisNoncapsular joint upper limb (Adhesive capsulitis of shoulder, Impingement syndrome Rotator cuff tear, Golfer's elbow, Tennis elbow)lower limb (Iliotibial band syndrome, Patellar tendinitis, Achilles tendinitis, Calcaneal spur, Metatarsalgia) · Bone spurNonjoint M: JNT
anat(h/c, u, t, l)/phys
noco(arth/defr/back/soft)/cong, sysi/epon, injr
proc, drug(M01C, M4)
Categories:- Overuse injuries
- Disorders of synovium and tendon
Wikimedia Foundation. 2010.