- Cochlear implant
-
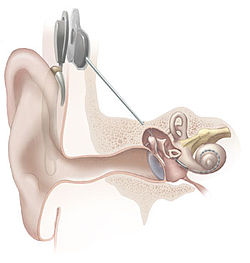
A cochlear implant (CI) is a surgically implanted electronic device that provides a sense of sound to a person who is profoundly deaf or severely hard of hearing. The cochlear implant is often referred to as a bionic ear.
As of December 2010, approximately 219,000 people worldwide have received cochlear implants; in the United States, roughly 42,600 adults and 28,400 children are recipients.[1] The vast majority are in developed countries due to the high cost of the device, surgery and post-implantation therapy. A small but growing segment of recipients have bilateral implants (one implant in each cochlea).[2]
Cochlear implants can restore hearing in patients suffering deafness due to loss of sensory hair cells in their cochlea. In those patients, they can often restore sufficient hearing to allow unaided understanding of speech in a quiet background, but the restored, electrical hearing is much less rich than natural hearing, and offers only very limited appreciation of musical melody, or speech understanding in noisy environments.
History
The discovery that electrical stimulation in the auditory system can create a perception of sound occurred around 1790, when Alessandro Volta (the developer of the electric battery) placed metal rods in his own ears and connected them to a 50-volt circuit, experiencing a jolt and hearing a noise "like a thick boiling soup". Other experiments occurred sporadically, until electrical (sound-amplifying) hearing aids began to be developed in earnest in the 20th century.
The first direct stimulation of an acoustic nerve with an electrode was performed in the 1950s by the French-Algerian surgeons André Djourno and Charles Eyriès. They placed wires on nerves exposed during an operation, and reported that the patient heard sounds like "a roulette wheel" and "a cricket" when a current was applied.
The first attempt to develop a clinical CI was in 1957 by Djourno and Eyriès. A recipient was implanted with a single channel device. Unprocessed sounds were transmitted via a pair of solenoid-like coils. The link was therefore transcutaneous; it did not require a break in the skin after implantation. This device failed after a short time and another device was implanted. After this second device failed, Eyriès refused to implant a third device. He urged Djourno to collaborate with an industry partner to build a more reliable device. Djourno refused because he believed that academia should not be tainted by commerce. Djourno found another surgeon, Roger Maspétiol, who implanted a second patient in 1958. Although these recipients were unable to understand speech with the device alone, it helped with lipreading by providing the rhythm of the speech.[citation needed]
In 1961 Dr William House (an otologist), John Doyle (a neurosurgeon) and James Doyle (an electrical engineer) commenced work on a single-channel device in Los Angeles. In one case a five-wire electrode was used but the same signal was applied to all contacts. House’s work continued in the 1970s in collaboration with engineer Jack Urban. Their implant was also a single-channel device but, in this case, the speech was modulated onto a carrier of 16 kHz. The device, manufactured by 3M, was ultimately implanted in some thousand or so recipients and paved the way for future clinical development of multichannel CIs.[3] The House/3M unit was the first approved by the FDA for implantation in adults in 1984.
In 1964, Blair Simmons at Stanford University implanted some recipients with a six-channel device. This device used a percutaneous plug to enable the electrodes to be individually stimulated. Recipients could still not understand speech through the device but, importantly, it demonstrated that by stimulating in different areas of the cochlea different pitch percepts could be produced.[4]
In 1970, Robin Michelson, M.D. reported preliminary results of cochlear implantation in three deaf adults implanted with gold wire electrodes. Initially he teamed with Mel Bartz, an electrical engineer working with Storz, Inc. Michelson's report to the American Academy of Otolaryngology and Ophthalmology created a tempest. Orthodox auditory theory was in confusion at the time, and it was not thought possible for direct electrical stimulation of neural tissue to convey meaningful sound to the brain. Michelson conducted some work in San Francisco, in the Coleman Laboratory at the University of California, a foundation funded by the wealthy ENT department chairman at UCSF, Francis Sooy, MD. Michelson's implantation of humans before animal physiology experiments caused consternation among physiologists, audiologists, and many otologists; his veracity and professional ethics were questioned, and the matter became a concern to the ENT department. An otolaryngology resident, C. Robert Pettit, heard Michelson describe the results of his cochlear implantations at a department educational meeting. He ran to the Coleman Laboratory, where Michelson spent one half-day per week away from his Redwood City private ENT practice, and told the older surgeon of his dream since college of a multi-channel electrode resembling a hairbrush. Michelson said so many stimulus points were not necessary and that his patients were hearing "in stereo" with a two-channel electrode he had designed. Michelson and Pettit teamed to build the bipolar electrodes embedded in silastic which replaced the broken gold electrodes in Michelson's three patients. The reimplantation procedures were carried out in Redwood City Community Hospital, not at UC San Francisco, as were the original implants.
When Michelson reported initial results of the reimplantation, in 1971, another hue and outcry arose: He was accused of lying about results and of unethical human experimentation. Michelson could not bring his brainchild to the university setting yet. Pettit was incensed when he witnessed Michelson's humiliation at the meeting. He had assisted in the reimplantation surgeries and witnessed the fact that the patients, when tested on the operating room table, could hear something meaningful. He decided to document on film the results of testing on the reimplanted patients to prove to the scientific community that electrical stimulation could result in meaningful sound perception.
Soon, the UCSF department chairman, recruited Michael Merzenich, a young PhD, to carry out his research interests in neurophysiology, mapping the inferior colliculus, and to investigate the potential of cochlear implantation. Merzenich was enormously skeptical of the cochlear implant project but agreed to test cats Michelson and Pettit had implanted. Merzenich was skilled at constructing micro-electrode needles capable of penetrating single nerve cells without rupturing the cell membranes and spilling cell contents. He agreed to monitor electrical activity in inferior colliculus cells of cats stimulated by normal sound in one ear, and electrical input from a cochlear implant in the other ear, finding both auditory stimuli similar. Merzenich had constructed an advanced electronic bank of signal generating and monitoring equipment for use for in his mapping experiments and a carefully shielded soundproof booth for testing. Over the months of animal testing, Merzenich became convinced that the electrical signal from the cochlear implant was entering the brain and was "phase-locked." Understanding what humans heard with the cochlear implant was another matter.
New tests were devised for implanted patients. One was congenitally deaf and had never heard sound. Pettit employed a music professor to synthesize simple tunes and sounds in various sound envelopes, and new pitch and loudness-scaling tests were devised. When one of the reimplanted patients was tested by the team under carefully controlled laboratory conditions, in 1972, a version of "Where Have All the Flowers Gone?" played on a Moog Synthesizer was presented to the patient through the cochlear implant. The camera caught the patient humming the melody and tapping a pencil to the tempo of the tune. That sequence convinced the department chairman to support the cochlear implant project. When the film was shown to a meeting of otologists later in 1972 it convinced the scientific community that meaningful sound could be conveyed to the brain by electrical stimulation of the auditory nerve.[5][6]
Cochlear implants that operate successfully, including those produced by all three major manufacturers (Cochlear Americas, Advanced Bionics and Med-El), incorporate the same basic design. Likewise, all cochlear implants incorporate the same basic design to be capable of the ultimate goal of "detecting" or "demodulating" intelligence from the human voice when that intelligence is residing within an electronic signal. The successful cochlear implant must also be capable of converting the pattern of the detected intelligence into an appropriate electronic format for application to the acoustic (eighth cranial) nerve, which in turn further transmits the encoded pattern to the hearing center of the brain, where the information is interpreted as meaningful intelligence. That is why implants from all (three) major manufacturers work equally well in functionality, but are quite different in final design enhancements. Design of this basic conversion process was first described by Adam Kissiah, Jr and was first exposed to the public when it was revealed to James O. Harrell, Esquire, Patent Counsel to NASA's John F. Kennedy Space Center, in July, 1974. Mr. Harrell also advised exposure to another person capable of understanding the concept. This was done on August 1, 1974. Subsequent Patent Office search and patent application for letters patent was completed in May, 1977. Patent 4063048 was issued to Adam M. Kissiah, Jr. on December 13, 1977; Reissue 31031, which further improved design, was issued on September, 1982.
Some cochlear implant designs and intra-cochlear implantations were made by others (see Cochlear Technology by Adam M. Kissiah, Jr.) prior to the mid-1970s, and were considered "successful" from a surgical and medical point of view. An equal number of proclamations and claims of being "firsts" in cochlear implantation were also made. Indeed, many important advances in cochlear implantation were accomplished during the 1960s and 70s. These earlier implants were capable of providing background sounds, and provided some aid to lip reading, and thus enabled patients to attain a most welcome sense of "attachment" to the world of sound. These earlier implants were incapable, however, of providing the ultimate level of comprehension of the intelligence of the spoken human voice enjoyed by the implant users of today. This fact can be supported by review of the many volumes of quarterly reports provided by many researchers under contract to the National Institutes of Health.
Greater understanding of voice intelligence was accomplished as the designs described in this first patent for the Cochlear Implant (4063048, December 13, 1977) were utilized in subsequent cochlear implants. Although Adam Kissiah was a full time employee with NASA at the Kennedy Space Center, he participated as a consultant in an implantation program during the early 1980s through license agreement granted by Kissiah to Biostim, Inc., who in turn participated (also by contractual agreement) with Stanford University, Dr. Robert L. White and Dr. F Blair Simmons, principal investigators, during their program of cochlear implants (See Stanford University Cochlear Implant Program).
In 1976 a paper (received Feb 1975) was published by Pialoux, Chouard and McLeod that stated that, in the six months before the paper being submitted, seven patients were implanted with an eight-channel device.[7] Although it was reported that about 50% of ordinary words were understood without lipreading, this has not been supported by audiological data in the literature.
In 1972 the House 3M single-electrode implant was the first to be commercially marketed.[8] However, it was Dr. Michelson's patents and ultimately device which are thought of as the first cochlear implants.[9]
Parallel to the developments in California, in the 1970s there were two other groups working on the development of the cochlear implant in Vienna, Austria and Melbourne, Australia. On December 16, 1977 professor Kurt Burian implanted a multichannel cochlear implant. The device was developed by the scientists Ingeborg and Erwin Hochmair, who founded MED-EL, producer of hearing implants, in 1989.[10]
Professor Graeme Clark A.C., then Foundation Professor of the Department of Otolaryngology at the University of Melbourne in 1970, led the team that developed the Australian prototype bionic ear, which was implanted into the first patient, Rod Saunders, in 1978.
The prototype for the bionic ear developed by Professor Clark can be seen at the National Museum of Australia in Canberra, Australia. It is part of a collection acquired by the National Museum in 2009 and includes key elements that figured in the development of the bionic ear, including the prototype multi-channel cochlear implant received by Rod Saunders in 1978 (subsequently removed when it was replaced by an updated model).[11]
In December 1984, the Australian cochlear implant was approved by the United States Food and Drug Administration to be implanted in adults in the United States. In 1990 the FDA lowered the approved age for implantation to two years, then 18 months in 1998, and finally 12 months in 2000,[12] although off-label use has occurred in babies as young as 6 months in the United States and 4 months internationally.[citation needed]
Throughout the 1990s, the large external components which had been worn strapped to the body grew smaller and smaller thanks to developments in miniature electronics. By 2006, most school-age children and adults used a small behind-the-ear (BTE) speech processor about the size of a power hearing aid. Younger children have small ears and might mishandle behind-the-ear speech processors, therefore, they often wear the sound processor on their hip in a pack or small harness or wear the BTEs pinned to their collar, barrette or elsewhere.
On October 5, 2005, the first of three recipients was implanted with Cochlear's TIKI device, a totally implantable cochlear implant, in Melbourne, Australia.[13] This was part of a research project conducted by Cochlear Ltd and the University of Melbourne Department of Otolaryngology under the umbrella of CRC HEAR to be the first cochlear implant system capable of functioning for sustained periods with no external components. The system is capable of providing hearing via the TIKI device in stand-alone mode (invisible hearing) or via an external sound processor. Although these recipients continue to use their devices successfully today, it will be many years before a commercial product becomes available.[14]
Since hearing in two ears allows people to localize sounds (given synchronised AGCs) and to hear better in noisy environments, bilateral (both ear) implants are being investigated and used. Users generally report better hearing with two implants, and tests show that bilateral implant users are better at localizing sounds and hearing in noise.[15] However, there is also evidence to suggest that the combination of one implant with an FM system provides better speech recognition in noise than two implants alone.[16] Additionally, dynamic FM technology has been proven to outperform traditional FM when used with cochlear implants. [17]
Nearly 3,000 people worldwide are bilateral cochlear implant users, including 1,600 children.[citation needed] As of 2006[update], the world's youngest recipient of a bilateral implant was just over 5 months old (163 days) in Germany (2004).[18]
Parts of the cochlear implant
The implant is surgically placed under the skin behind the ear. The basic parts of the device include:
- External:
- one or more microphones which picks up sound from the environment
- a speech processor which selectively filters sound to prioritize audible speech splits the sound into channels and sends the electrical sound signals through a thin cable to the transmitter,
- a transmitter, which is a coil held in position by a magnet placed behind the external ear, and transmits power and the processed sound signals to the internal device by electromagnetic induction,
- Internal:
- a receiver and stimulator secured in bone beneath the skin, which converts the signals into electric impulses and sends them through an internal cable to electrodes,
- an array of up to 24 electrodes wound through the cochlea, which send the impulses to the nerves in the scala tympani and then directly to the brain through the auditory nerve system. There are 4 manufacturers for Cochlear implants, and each one produces a different implant with a different number of electrodes. The number of channels is not a primary factor upon which a manufacturer is chosen; the signal processing algorithm is also another important block.
Candidates
There are a number of factors that determine the degree of success to expect from the operation and the device itself. Cochlear implant centers determine implant candidacy on an individual basis and take into account a person's hearing history, cause of hearing loss, amount of residual hearing, speech recognition ability, health status, and family commitment to aural habilitation/rehabilitation.
A prime candidate is described as:
- having severe to profound sensorineural hearing impairment in both ears.
- having a functioning auditory nerve
- having lived at least a short amount of time without hearing (approximately 70+ decibel hearing loss, on average)
- having good speech, language, and communication skills, or in the case of infants and young children, having a family willing to work toward speech and language skills with therapy
- not benefitting enough from other kinds of hearing aids, including latest models of high power hearing instruments and FM systems
- having no medical reason to avoid surgery
- living in or desiring to live in the "hearing world"
- having realistic expectations about results
- having the support of family and friends
- having appropriate services set up for post-cochlear implant aural rehabilitation (through a speech language pathologist, deaf educator, or auditory verbal therapist).
Type of hearing impairment
People with mild or moderate sensorineural hearing loss are generally not candidates for cochlear implantation. Their needs can often be met with hearing aids alone or hearing aids with an FM system. After the implant is put into place, sound no longer travels via the ear canal and middle ear but will be picked up by a microphone and sent through the device's speech processor to the implant's electrodes inside the cochlea. Thus, most candidates have been diagnosed with profound sensorineural hearing loss.
The presence of auditory nerve fibers is essential to the functioning of the device: if these are damaged to such an extent that they cannot receive electrical stimuli, the implant will not work. A small number of individuals with severe auditory neuropathy may also benefit from cochlear implants.
Age of recipient
Post-lingually deaf adults, pre-lingually deaf children and post-lingually impaired people (usually children) who have lost hearing due to diseases such as meningitis, form three distinct groups of potential users of cochlear implants with different needs and outcomes. Those who have lost their hearing as adults were the first group to find cochlear implants useful, in regaining some comprehension of speech and other sounds. If an individual has been deaf for a long period of time, the brain may begin using the area of the brain typically used for hearing for other functions. If such a person receives a cochlear implant, the sounds can be very disorienting, and the brain often will struggle to readapt to sound.
The risk of surgery in the older patient must be weighed against the improvement in quality of life. As the devices improve, particularly the sound processor hardware and software, the benefit is often judged to be worth the surgical risk, particularly for the newly deaf elderly patient.[19]
Another group of customers are parents of children born deaf who want to ensure that their children grow up with good spoken language skills. Research shows that congenitally deaf children who receive cochlear implants at a young age (less than 2 years) have better success with them than congenitally deaf children who first receive the implants at a later age, though the critical period for utilizing auditory information does not close completely until adolescence. Additionally, a 2010 study into bilateral implantation showed that children who receive their first cochlear implant before the age of 1½ responded well to the second one, even if the second one was implanted as late as 9 years old. In contrast, children who got their implants at age 2½ years or later did not respond as well to the later second implant, regardless of when they received it.[20] One doctor has said "There is a time window during which they can get an implant and learn to speak. From the ages of two to four, that ability diminishes a little bit. And by age nine, there is zero chance that they will learn to speak properly. So it’s really important that they get recognized and evaluated early."[21]
The third group who will benefit substantially from cochlear implantation are post-lingual subjects who have lost hearing: a common cause is childhood meningitis. Young children (under five years) in these cases often make excellent progress after implantation because they have learned how to form sounds, and only need to learn how to interpret the new information in their brains.
Number of users
It was estimated in 2002 that around 10,000 children in the US and an additional 49,000 people worldwide had received Cochlear implants. By the end of 2008, the total number of cochlear implant recipients has grown to an estimated 150,000 worldwide.[22] A story in 2000 stated that one in ten deaf children in the United States had a cochlear implant, and that the projection was the ratio would rise to one in three in ten years.[23]
Mexico had performed only 55 cochlear implant operations by the year 2000 (Berruecos 2000). Taiwan and China announced an approximately $270 million order for cochlear implant devices for children in 2006, which are being paid for by major healthcare organization based in Taipei. These cochlear implants are a donation by the Taiwanese organization[24][25]
In India, there are an estimated 1 million profoundly deaf children, only about 5,000 have cochlear implants. This minuscule number is due to the high costs for the implant, as well as subsequent therapy.[26]
The operation, post-implantation therapy and ongoing effects
The device is surgically implanted under a general anesthetic, and the operation usually takes from 1½ to 5 hours. First a small area of the scalp directly behind the ear is shaved and cleaned. Then a small incision is made in the skin just behind the ear and the surgeon drills into the mastoid bone and the inner ear where the electrode array is inserted into the cochlea. The patient normally goes home the same day or the day after the surgery, although some cochlear implant recipients stay in the hospital for 1 to 2 days. It is considered outpatient surgery. As with every medical procedure, the surgery involves a certain amount of risk; in this case, the risks include skin infection, onset of (or change in) tinnitus, damage to the vestibular system, and damage to facial nerves that can cause muscle weakness, impaired facial sensation, or, in the worst cases, disfiguring facial paralysis. There is also the risk of device failure, usually where the incision does not heal properly. This occurs in 2% of cases and the device must be removed. The operation also destroys any residual hearing the patient may have in the implanted ear; as a result, some doctors advise single-ear implantation, saving the other ear in case a biological treatment becomes available in the future.
After 1–4 weeks of healing (the wait is usually longer for children than adults) during which the wound must be kept dry, the implant is turned on or "activated". Results are typically not immediate, and post-implantation therapy is required as well as time for the brain to adapt to hearing new sounds. In the case of congenitally deaf children, audiological training and speech therapy typically continue for years, though infants can become age appropriate—able to speak and understand at the same level as a hearing child of the same age in a matter of months—however it is far more common for the process to take years. The participation of the child's family in working on spoken language development is considered to be even more important than therapy, because the family can aid development by participating actively—and continually—in the child's therapy, making hearing and listening interesting, talking about objects and actions, and encouraging the child to make sounds and form words. Professionals trained to work with children who have received cochlear implants are a major part of the parent-professional team when addressing the task of teaching children to use their hearing to develop speech and spoken language. These professionals include, but are not limited to:
- Speech-Language Pathologists (SLP)
- Certified Auditory-Verbal Therapists (LSLS Cert. AVT) A.G. Bell
- Pediatric Audiologist (AuD)
- Teacher of the Deaf (ToD) with a specialization in Oral Deaf Education
Many users, audiologists, and surgeons also report that when there is an ear infection causing fluid in the middle ear, it can affect the cochlear implant, leading to temporarily reduced hearing.
The implant has a few effects unrelated to hearing. Manufacturers have cautioned against scuba diving due to the pressures involved, but the depths found in normal recreational diving appear to be safe. The external components must be turned off and removed prior to swimming or showering. Some brands of cochlear implant are unsafe in areas with strong magnetic fields, and thus cannot be used with certain diagnostic tests such as magnetic resonance imaging (MRI), but some are now FDA approved for use with certain strengths of MRI machine. Large amounts of static electricity can cause the device's memory to reset. For this reason, children with cochlear implants are also advised to avoid plastic playground slides.[27] The electronic stimulation the implant creates appears to have a positive effect on the nerve tissue that surrounds it.[28]
Cost
In the United States, medical costs run from US$45,000 to US$125,000; this includes evaluation, the surgery itself, hardware (device), hospitalization and rehabilitation. Some or all of this may be covered by health insurance. In the United Kingdom, the NHS covers cochlear implants in full, as does Medicare in Australia, Seguridad Social in Spain and Israel. According to the US National Institute on Deafness and Other Communication Disorders, the estimated total cost is $60,000 per person implanted.
A study by Johns Hopkins University determined that for a three-year-old child who receives cochlear implants can save $30,000 to $50,000 in special-education costs for elementary and secondary schools as they are more likely to be mainstreamed in school and thus use fewer support services than similarly deaf children.[29]
Efficacy
A cochlear implant will not cure deafness or hearing impairment, but is a prosthetic substitute for hearing. Some[quantify] recipients find them very effective, others[quantify] somewhat effective and some[quantify] feel worse overall with the implant than without.[30] For people already functional in spoken language who lose their hearing, cochlear implants can be a great help in restoring functional comprehension of speech, especially if they have only lost their hearing for a short time.
Individuals who have acquired deafblindness (loss of hearing and vision combined) may find cochlear implants a radical improvement in their daily lives. It may provide them with more information for safety, communication, balance, orientation and mobility and promote interaction within their environment and with other people, reducing isolation. Having more auditory information than they may be familiar with may provide them with sensory information that will help them become more independent.
British Member of Parliament Jack Ashley received a cochlear implant in 1994 at age 70 after 25 years of deafness, and reported that he has no trouble speaking to people he knows; whether one on one or even on the telephone, although he might have difficulty with a new voice or with a busy conversation, and still had to rely to some extent on lip reading. He described the robotic sound of human voices perceived through the cochlear implant as "a croaking dalek with laryngitis". Another recipient described the initial sounds as similar to radio static and voices as being cartoonish, though after a year with the implant she said everything sounded right.[31] Even modern cochlear implants have at most 24 electrodes to replace the 16,000 delicate hair cells that are used for normal hearing. However, the sound quality delivered by a cochlear implant is often good enough that many users do not have to rely on lip reading in quiet conditions. In noisy conditions however, speech understanding often remains poor.[32]
Adults who have grown up deaf can find the implants ineffective or irritating. This relates to the specific pathology of deafness and the time frame. Adults who are born with normal hearing and who have had normal hearing for their early years and who have then progressively lost their hearing tend to have better outcomes than adults who were born deaf. This is due to the neural patterns laid down in the early years of life, which are crucially important to speech perception. Cochlear implants cannot overcome such a problem. Some who were orally educated and used amplifying hearing aids have been more successful with cochlear implants, as the perception of sound was maintained through use of the hearing aid.
Children without a working auditory nerve may be helped with a cochlear implant, although the results may not be optimal. Patients without a viable auditory nerve are usually identified during the candidacy process. Fewer than 1% of deaf individuals have a missing or damaged auditory nerve, which today can be treated with an auditory brainstem implant. Research published in 2005 has suggested that children and adults can benefit from bilateral cochlear implants in order to aid in sound localization and speech understanding,[33] and a 2011 study indicated that the language skills of children with two implants was within the normal range for the age.[34]
Risks and disadvantages
Some effects of implantation are irreversible; while the device promises to provide new sound information for a recipient, the implantation process inevitably results in shaving of the hair cells within the cochlea,[35] which can result in a permanent loss of most residual natural hearing because sometimes the cause of deafness is the auditory nerve or other part of the body. While recent improvements in implant technology, and implantation techniques, promise to minimize such damage, the risk and extent of damage still varies. Still, the cause of deafness is not always identified before the surgery. It is quite possible that the surgery does not restore hearing.
In addition, while the device can help the recipient better hear and understand sounds in their environment, it is not as good as the quality of sound processed by a natural cochlea. The main problem is with the age of recipient. While cochlear implants restore physical ability to hear, this does not mean the brain can learn to process and distinguish speech if the recipient has passed the critical period of adolescence. As a result, those born profoundly deaf who receive an implant as an adult can only distinguish simple sounds,[citation needed] such as a ringing phone vs. a doorbell, while others who receive implants early can understand speech.[citation needed] The success rate depends on a variety of factors, most critically the age of recipient but also the technology used and the condition of the recipient's cochlea.
The United States Food and Drug Administration reports that cochlear implant recipients may be at higher risk for meningitis.[36] A study of 4,265 American children who received implants between 1997 and 2002 concluded that recipient children had a risk of pneumococcal meningitis more than 30 times greater than that for children in the general population.[37] A later, UK-based, study found that while the incidence of meningitis in implanted adults was significantly higher than the general population, the incidence in children was no different than the general population.[38] As a result, the Centers for Disease Control and Prevention and the Food and Drug Administration both recommend that would-be implant recipients be vaccinated against meningitis prior to surgery.[39]
Necrosis has been observed in the skin flaps surrounding cochlear implants.[40][41] Hyperbaric oxygen has been shown to be a useful adjunctive therapy in the management of cochlear implant flap necrosis.[42]
As the location of the cochlea is close to the facial nerve, there is a risk that the nerve may be damaged during the operation. The incidence of the damage is infrequent.[43]
There are strict protocols in choosing candidates to avoid risks and disadvantages. A battery of tests is performed to make the decision of candidacy easier. For example, some patients suffer from deafness medial to the cochlea - typically vestibular schwannomas. Implantation into the cochlea has a low success rate with these people, as the artificial signal does not have a healthy nerve to travel along.
With careful selection of candidates, the risks of implantation are minimized.
Functionality
The implant works by using the tonotopic organization of the basilar membrane of the inner ear. "Tonotopic organization", also referred to as a "frequency-to-place" mapping, is the way the ear sorts out different frequencies so that our brain can process that information. In a normal ear, sound vibrations in the air lead to resonant vibrations of the basilar membrane inside the cochlea. High-frequency sounds (i.e. high pitched sounds) do not pass very far along the membrane, but low frequency sounds pass farther in. The movement of hair cells, located all along the basilar membrane, creates an electrical disturbance that can be picked up by the surrounding nerve cells. The brain is able to interpret the nerve activity to determine which area of the basilar membrane is resonating, and therefore what sound frequency is being heard.
In individuals with sensorineural hearing loss, hair cells are often fewer in number and damaged. Hair cell loss or absence may be caused by a genetic mutation or an illness such as meningitis. Hair cells may also be destroyed chemically by an ototoxic medication, or simply damaged over time by excessively loud noises. The cochlear implant bypasses the hair cells and stimulates the cochlear nerves directly using electrical impulses. This allows the brain to interpret the frequency of sound as it would if the hair cells of the basilar membrane were functioning properly (see above).
Processing
Sound received by the microphone must next be processed to determine how the electrodes should be activated.
Filterbank strategies use Fast Fourier Transforms to divide the signal into different frequency bands. The algorithm chooses a number of the strongest outputs from the filters, the exact number depending on the number of implanted electrodes and other factors. These strategies emphasize transmission of the spectral aspects of speech. Although coarse temporal information is presented, the fine timing aspects are as yet poorly perceived and this is the focus of much current research.
Feature extraction strategies used features which are common to all vowels. Each vowel has a fundamental frequency (the lowest frequency peak) and formants (peaks with higher frequencies). The pattern of the fundamental and formant frequencies is specific for different vowel sounds. These algorithms try to recognize the vowel and then emphasize its features. These strategies emphasize the transmission of spectral aspects of speech. Feature extraction strategies are no longer widely used. Each Cochlear implant manufacturer tries to use a different strategy, Cochlear - 70% market share- for example uses the Speak-ACE strategy, ACE is mainly used; in which number of maxima (n) from the available maxima in sound are selected, Advanced Bionics uses other techniques like CIS, SAS and HiRes, they stimulate the full spectrum. The processing strategy is a main block upon which one has to choose the implant manufacturer, research shows that patients can understand speech with at least 4 electrodes, but the obstacle is in music perception, where it returns that fine structure stimulation is an important issue. Some strategies used in Advanced Bionics and MED-EL strategies make use of fine structure presentation by implementing the Hilbert Transform in the signal processing path, while ACE strategies depends mainly on the Short Time Fourier Transform.
Transmitter
This is used to transmit the processed sound information over a radio frequency link to the internal portion of the device. Radio frequency is used so that no physical connection is needed, which reduces the chance of infection and pain. The transmitter attaches to the receiver using a magnet that holds through the skin.
Receiver
This component receives directions from the speech processor by way of magnetic induction sent from the transmitter. (The receiver also receives its power through the transmission.) The receiver is also a sophisticated computer that translates the processed sound information and controls the electrical current sent to the electrodes in the cochlea. It is embedded in the skull behind the ear.
Electrode array
The electrode array is made from a type of silicone rubber, while the electrodes are platinum or a similar highly conductive material. It is connected to the internal receiver on one end and inserted into the cochlea deeper in the skull. (The cochlea winds its way around the auditory nerve, which is tonotopically organized as is the basilar membrane). When an electrical current is routed to an intracochlear electrode, an electrical field is generated and auditory nerve fibers are stimulated.
In the devices manufactured by Cochlear Ltd, two electrodes sit outside the cochlea and act as grounds-- one is a ball electrode that sits beneath the skin, while the other is a plate on the device. This equates to 24 electrodes in the Cochlear-brand 'nucleus' device, 22 array electrodes within the cochlea and 2 extra-cochlear electrodes.
Insertion depth is another important factor. The mean length of human being cochlea is 33–36 mm, due to some physical limitation, the implants don't reach to the apical tip when inserted but it may reach up to 25 mm which corresponds to a tonotopical frequency of 400–6000 Hz. MED-EL produces deep insertion implants that can be inserted up to a tonotopical frequency of 100 Hz (according to Greenwood frequency to position formula in normal hearing), but the distance between the electrodes is about 2.5 mm, while in the Nucleus Freedom from Cochlear Ltd is about 0.7 mm. There is a strong research in this direction and the best sounding implant can be subjective from patient to patient.
Speech processors
Speech processors are the components of the cochlear implant that transforms the sounds picked up by the microphone into electronic signals capable of being transmitted to the internal receiver. The coding strategies programmed by the user's audiologist are stored in the processor, where it codes the sound accordingly. The signal produced by the speech processor is sent through the coil to the internal receiver, where it is picked up by radio signal and sent along the electrode array in the cochlea.
There are primarily two forms of speech processors available. The most common kind is called the "behind-the-ear" processor, or BTE. It is a small processor that is worn on the ear, typically together with the microphone. This is the kind of processor used by most adults and older children. Babies and small children wear either a "baby" BTE (pinned or clipped to the collar) or the body-worn processor, which was more common in previous years. Today's tiny processors can often take the place of bulky body-worn processors. MED-EL and Cochlear brands both carry a "baby BTE" configurations.
Programming the speech processor
The audiologist sets the minimum and maximum current level outputs for each electrode in the array based on the user's reports of loudness. The audiologist also selects the appropriate speech processing strategy and program parameters for the user.
Scientific and technical advances
Professor Graeme Clark A.C. of La Trobe University, Melbourne, Australia, in 2008, announced beginning the development of a prototype "hi fi" cochlear implant featuring 50 electrodes. It is hoped that the increased number of electrodes will enable users to perceive music and discern specific voices in noisy rooms.[44]
Researchers at Northwestern University have used infrared light to directly stimulate the neurons in the inner ear of deaf guinea pigs while recording electrical activity in the inferior colliculus, an area of the midbrain that acts as a bridge between the inner ear and the auditory cortex. The laser stimulation produced more precise signals in that brain region than the electrical stimulation commonly used in cochlear implants.[45] Laser stimulation is a promising technology for improving the auditory resolution of implants but further research using fiber optics to stimulate the neurons of the inner ear is required before products using the technology can be developed.
Cochlear implants are rarely used in ears that have a functional level of residual hearing. However, Electric Acoustic Stimulation (EAS) devices, including the Hybrid "short-electrode" cochlear implant, have been developed that combine a cochlear implant with a sound amplifying hearing aid.[46][47] EAS devices have the potential to make cochlear implants suitable for many people with partial hearing loss. The sound amplifying component helps users to perceive lower frequency sounds through their residual natural hearing while the cochlear implant allows them to hear middle and higher frequency sounds. The combination enhances speech perception in noisy environments.[48]
Additionally, work is ongoing in developing a fully internal cochlear implant. As of April 2011, four people have undergone a trial of an internal microphone system, with two more yet to come.[49]
Manufacturers
Currently (as of 2007[update]), the three cochlear implant devices approved for use in the U.S. are manufactured by Cochlear Limited, Australia, Advanced Bionics, US and MED-EL, Austria. In the EU, an additional device manufactured by Neurelec, of France, is available. Each manufacturer has adapted some of the successful innovations of the other companies to its own devices. There is no clear-cut consensus that any one of these implants is superior to the others. Users of all four devices display a wide range of performance after implantation.
Since the devices have a similar range of outcomes, other criteria are often considered when choosing a cochlear implant: FM system compatibility, usability of external components, cosmetic factors, battery life, reliability of the internal and external components, MRI compatibility, mapping strategies, customer service from the manufacturer, the familiarity of the user's surgeon and audiologist with the particular device, and anatomical concerns.
There have been news reports of other organizations working to develop cochlear implants, in South Korea by the Seoul National University Hospital[50] and in India by a branch of the Defence Research and Development Organisation.[51]
Controversy in Deaf culture
Much of the strongest objection to cochlear implants has come from the Deaf community, which consists largely of pre-lingually deaf people whose first language is a signed language. For some in the Deaf community, cochlear implants are an affront to their culture, which as they view it, is a minority threatened by the hearing majority.[52] This is an old problem for the Deaf community, going back as far as the 18th century with the argument of manualism vs. oralism.
Cochlear implants for congenitally deaf children are considered to be most effective when implanted at a young age, during the critical period in which the brain is still learning to interpret sound.[21] Hence they are implanted before the recipients can decide for themselves, on the assumption that deafness is a disability. Deaf culture critics argue that the cochlear implant and the subsequent therapy often become the focus of the child's identity at the expense of a possible future Deaf identity and ease of communication in sign language, and claim that measuring the child's success only by their mastery of hearing and speech will lead to a poor self-image as "disabled" (because the implants do not produce normal hearing) rather than having the healthy self-concept of a proudly Deaf person.[53]
Children with cochlear implants are more likely to be educated orally, in the standard fashion, and without access to sign language (Spencer et al. 2003). They are often isolated from other deaf children and from sign language (Spencer 2003). Children do not always receive support in the educational system to fulfill their needs as they may require special education environments and Educational Assistants. According to Johnston (2004), cochlear implants have been one of the technological and social factors implicated in the decline of sign languages in the developed world. Some of the more extreme responses from Deaf activists have labeled the widespread implantation of children as "cultural genocide".[23] Andrew Solomon of the New York Times states that "Much National Association of the Deaf propaganda about the danger of implants is alarmist; some of it is positively inaccurate."[54]
Opposition continues today but is softening. As the trend for cochlear implants in children grows, deaf-community advocates have tried to counter the "either or" formulation of oralism vs manualism with a "both and" approach; some schools now are successfully integrating cochlear implants with sign language in their educational programs. However, some opponents of sign language education argue that the most successfully implanted children are those who are encouraged to listen and speak rather than overemphasize their visual sense.
See also
- Auditory brainstem implant
- Brain implant
- Electric Acoustic Stimulation
- Neuroprosthetics
- Noise health effects
- Hearing Aid
- Bone conduction
References
- ^ NIH Publication No. 11-4798 (2011-03-01). "Cochlear Implants". National Institute on Deafness and Other Communication Disorders. http://www.nidcd.nih.gov/health/hearing/pages/coch.aspx. "as of December 2010, approximately 219,000 people worldwide have received implants. In the United States, roughly 42,600 adults and 28,400 children have received them."
- ^ Ahmed, Nabila (2007-02-14). "Cochlear heads for earnings record". The Age. http://www.theage.com.au/news/business/cochlear-heads-for-earnings-record/2007/02/13/1171128974085.html#. Retrieved 2008-04-27.
- ^ W.F. House (May–June 1976). "Cochlear implants". Annals of Otology, Rhinology and Laryngology 85 (suppl 27) (3Pt2): 1–93. PMID 779582.
- ^ F. Blair Simmons (July 1966). "Electrical Stimulation of the Auditory Nerve in Man". Archives of Otolaryngology 84 (1): 2–54. PMID 5936537.
- ^ References: Michelson RP, Merzenich MM,Pettit, Schindler RAc, "A cochlear prosthesis: Further clinical observations; preliminary results of physiological studies," presented at the Meeting of the Western Section of the American Laryngological, Rhinological and Otological Society, Inc., Pebble Beach, Calif., February 2, 1973.
- ^ Waltzman, SB, Roland, TJ, Cochlear Implants, 2nd edition, Chapter 1, pp1-10
- ^ P. Pialoux?, C. H. Chouard? and P. Macleod? (1976). "Physiological and Clinical Aspects of the Rehabilitation of Total Deafness By Implantation of Multiple Intracochlear Electrodes". Acta Oto-laryngologica 81 (3-6): 436–441. PMID 1274555.
- ^ "History of Cochlear Implants". http://biomed.brown.edu/Courses/BI108/BI108_2001_Groups/Cochlear_Implants/history.html.
- ^ See Robin Michelson's patents here: Patent Patent 2.3M Power Point Presentation on the Cochlear Implant.
- ^ Burian K, Hochmair E, Hochmair-Desoyer IJ. Lesser MR (1979)
- ^ http://nma.gov.au/collections/bionic_ear_prototype/
- ^ http://www.nidcd.nih.gov/health/hearing/coch.html#c
- ^ Briggs, RJ; HC Eder, PM Seligman, RS Cowan, KL Plant, J Dalton, DK Money, JF Patrick (2008-02). "Initial clinical experience with a totally implantable cochlear implant research device". Otology and Neurotology 29 (2): 114–119. doi:10.1097/MAO.0b013e31814b242f. PMID 17898671.
- ^ "The Cooperative Research Centre for Cochlear Implant and Hearing Aid Innovation: Annual Report 2006/2007" (PDF). http://www.medoto.unimelb.edu.au/crc/crc_hear_ar07.pdf. Retrieved 2008-04-27.[dead link]
- ^ Dave Tenenbaum (2010-01-11). "Study: Second cochlear implant can restore two important facets of binaural hearing". University of Wisconsin-Madison News. http://www.news.wisc.edu/17519. Retrieved 2010-01-12.
- ^ Erin C. Schafer, Linda M. Thibodeau (December 2006). "Speech Recognition in Noise in Children With Cochlear Implants While Listening in Bilateral, Bimodal, and FM-System Arrangements". American Journal of Audiology 15: 114–126.
- ^ Jace Wolfe, Erin C. Schafer, Benjamin Heldner, Hans Mülder, Emily Ward, Brandon Vincent (2009). "Evaluation of Speech Recognition in Noise with Cochlear Implants and Dynamic FM". Journal of the American Academy of Audiology 20: 409–421.
- ^ Mary Ann Moon. "Article: Cochlear implant is the first step in long journey.". Pediatric News. Archived from the original on 2002-05-01. http://www.accessmylibrary.com/coms2/summary_0286-90305_ITM. Retrieved 2010-01-25.
- ^ Shapiro, Joseph (2005-12-20). "Elderly with Hearing Loss Turning to Cochlear Implants". Day to Day (National Public Radio). http://www.npr.org/templates/story/story.php?storyId=5062928. Retrieved 2008-04-27.
- ^ "Success of Second Cochlear Implant Depends on Age at Which Child Receives First Implant" (Press release). National Institutes of Health. 2010-02-04. http://www.nih.gov/news/health/feb2010/nidcd-04.htm. Retrieved 2010-02-05.
- ^ a b Paul Oginni (2009-11-16). "UCI Research with Cochlear Implants No Longer Falling on Deaf Ears". New University. http://www.newuniversity.org/2009/11/news/uci-research-with-cochlear-implants-no-longer-falling-on-deaf-ears/. Retrieved 2009-11-18.
- ^ van der Heijden, Dennis (2006-03-01). "What are Cochlear Implants?". Axistive. http://www.axistive.com/what-are-cochlear-implants-.html. Retrieved 2007-03-01.
- ^ a b Amy E. Nevala (2000-09-28). "Not everyone is sold on the cochlear implant". Seattle Post-Intelligencer. http://www.seattlepi.com/lifestyle/cont28.shtml. Retrieved 2009-11-04.
- ^ "Cochlear Corp. News". http://www.cochlear.com/News/1810.asp.
- ^ "Cochlear Corp. News". http://www.cochlear.com/au/corporate/announces-order-china.
- ^ Priyanka Golikeri (2010-07-14). "Costly cochlear implants beyond reach of masses". dnaindia.com. http://www.dnaindia.com/money/report_costly-cochlear-implants-beyond-reach-of-masses_1409419. Retrieved 14 July 2010.
- ^ Dotinga, Randy (2006-08-06). "Slides: a playground menace". Wired. http://www.wired.com/medtech/health/news/2006/06/70937. Retrieved 2008-04-27.
- ^ Solomon, Andrew (1994-08-28). "Defiantly deaf". New York Times Magazine. http://query.nytimes.com/gst/fullpage.html?res=9A00E2D91639F93BA1575BC0A962958260&sec=&spon=&pagewanted=10. Retrieved 2008-04-27.
- ^ John M. Williams (2000-05-05). "Do Health-Care Providers Have to Pay for Assistive Tech?". Business Week. http://www.businessweek.com/bwdaily/dnflash/may2000/nf00505c.htm. Retrieved 2009-10-25.
- ^ Delost, Shelli; Sarah Lashley (2000-03). "The Cochlear Implant Controversy". Drury Interdisciplinary Research Conference. http://www.drury.edu/multinl/story.cfm?ID=2442&NLID=166. Retrieved 2008-04-27.
- ^ Rempp, Kerri (2009-06-11). "City clerk outsmarts heredity". The Chaldron Record. http://www.thechadronnews.com/articles/2009/06/11/chadron/headlines/doc4a1d6a310403c812363413.txt. Retrieved 2009-06-19.
- ^ Erin C. Schafer, Linda M. Thibodeau (2004). "Speech recognition abilities of adults using CIs interfaced with FM systems". Journal of the Amercian Academy of Audiology 15(10): 678–691.
- ^ Offeciers E, Morera C, Müller J, Huarte A, Shallop J, Cavallé L. (Sep 2005). "International consensus on bilateral cochlear implants and bimodal stimulation". Acta Otolaryngol. 125 (9): 918–919. doi:10.1080/00016480510044412. PMID 16109670.
- ^ Tenenbaum, David (2011-10-24). "Deaf children: Study shows significant language progress after two cochlear implants (Oct. 24, 2011)". news.wisc.edu. http://www.news.wisc.edu/19941. Retrieved 25 October 2011.
- ^ http://www.surgeryencyclopedia.com/Ce-Fi/Cochlear-Implants.html
- ^ "FDA Public Health Notification: Risk of Bacterial Meningitis in Children with Cochlear Implants". FDA. July 24, 2002. http://www.fda.gov/cdrh/safety/cochlear.html. Retrieved 2008-11-09.
- ^ Biernath, K. R.; Reefhuis, J; Whitney, CG; Mann, EA; Costa, P; Eichwald, J; Boyle, C. "Bacterial Meningitis Among Children With Cochlear Implants Beyond 24 Months After Implantation - Biernath et al. 117 (2): 284 - Pediatrics". Pediatrics 117 (2): 284. doi:10.1542/peds.2005-0824. PMID 16390918. http://pediatrics.aappublications.org/cgi/content/abstract/117/2/284. Retrieved 2008-11-09.
- ^ "Incidence of meningitis and of death from all causes among users of cochlear implants in the United Kingdom - Summerfield et al., 10.1093/pubmed/fdh188 - Journal of Public Hea...". doi:10.1093/pubmed/fdh188. http://jpubhealth.oxfordjournals.org/cgi/content/short/fdh188v1. Retrieved 2008-11-09.
- ^ "Maryland Hearing and Balance Center". University of Maryland Medical Center. http://www.umm.edu/otolaryngology/cochlear.htm#noF. Retrieved 2009-10-25.
- ^ Haberkamp TJ, Schwaber MK (January 1992). "Management of flap necrosis in cochlear implantation". Ann. Otol. Rhinol. Laryngol. 101 (1): 38–41. PMID 1728883.
- ^ Stratigouleas ED, Perry BP, King SM, Syms CA (September 2006). "Complication rate of minimally invasive cochlear implantation". Otolaryngol Head Neck Surg 135 (3): 383–6. doi:10.1016/j.otohns.2006.03.023. PMID 16949968. http://linkinghub.elsevier.com/retrieve/pii/S0194-5998(06)00371-8. Retrieved 2009-04-01.
- ^ Schweitzer VG, Burtka MJ (1990). "Hyperbaric Oxygen Therapy in the Management of Cochlear Implant Flap Necrosis.". J. Hyperbaric Med 5 (2): 81–90. http://archive.rubicon-foundation.org/4424. Retrieved 2009-04-01.
- ^ The Parents' Guide to Cochlear Implants. Gallaudet University Press. 2002. p. 44. ISBN 1-56368-129-3.
- ^ Cochlear implant maker says hi-fi bionic ear will help the deaf hear music. News.com.au, December 18, 2008.
- ^ Nowak, R. (2008). Light opens up a world of sound for the deaf. New Scientist.
- ^ UT Southwestern Medical Center (2008, April 28). New Hybrid Hearing Device Combining Advantages Of Hearing Aids, Implants. ScienceDaily. Retrieved December 22, 2008, from http://www.sciencedaily.com /releases/2008/04/080417100013.htm
- ^ Gantz, B.G. and Turner, C.W. (2004) Combining acoustic and electrical speech processing: Iowa/Nucleus hybrid implant. Acta Otolaryngol 124: 344-347. See also: http://www.nationalreviewofmedicine.com/issue/2006/03_30/3_advances_medicine02_6.html
- ^ Turner, C.W., Gantz, B.J., Vidal, C., et al. (2004) Speech recognition in noise for cochlear implant listeners: Benefits of residual acoustic hearing J. Acoust. Soc. Am. Volume 115, Issue 4, pp. 1729-1735.
- ^ Graham-Rowe, Duncan (2011-04-04). "Ear implants for the deaf with no strings attached - tech - 04 April 2011 - New Scientist". newscientist.com. http://www.newscientist.com/article/mg21028064.800-ear-implants-for-the-deaf-with-no-strings-attached.html. Retrieved 5 April 2011.
- ^ Bae Ji-sook (2010-02-28). "Procedure Gives Hearing to Auditory Disabled". The Korea Times. http://www.koreatimes.co.kr/www/news/art/2010/02/147_61550.html. Retrieved 2010-03-05.
- ^ "Cheaper, lighter biomedical equipment using Def-tech". Zee News. 2010-03-05. http://www.zeenews.com/news608563.html. Retrieved 2010-03-05.
- ^ "The Cochlear Implant Controversy, Issues And Debates". NEW YORK: CBS News. September 4, 2001. http://www.cbsnews.com/stories/1998/06/02/sunday/main10794.shtml. Retrieved 2008-11-09.
- ^ NAD Cochlear Implant Committee. "Cochlear Implants". Archived from the original on 2007-02-20. http://web.archive.org/web/20070220131900/http://www.nad.org/site/pp.asp?c=foINKQMBF&b=138140.
- ^ Solomon, Andrew (1994-08-28). "Defiantly deaf". The New York Times. http://query.nytimes.com/gst/fullpage.html?res=9A00E2D91639F93BA1575BC0A962958260&sec=health&pagewanted=10. Retrieved 2010-04-30.
Further reading
- Berruecos, Pedro. (2000). Cochlear implants: An international perspective - Latin American countries and Spain. Audiology. Hamilton: Jul/Aug 2000. Vol. 39, 4:221-225
- House, W. F., Cochlear Implants. Ann Otol Rhinol Larynogol 1976; 85 (suppl 27): 1 – 93.
- Simmons, F. B., Electrical Stimulation of the Auditory Nerve in Man, Arch Otolaryng, Vol 84, July 1966
- Pialoux, P., Chouard, C. H. and MacLeod, P. 1976. Physiological and clinical aspects of the rehabilitation of total deafness by implantation of multiple intracochlear electrodes. Acta Oto-Laryngologica 81: 436-441
- Chorost, Michael. (2005). Rebuilt: How Becoming Part Computer Made Me More Human. Boston: Houghton Mifflin.
- Christiansen, John B., and Irene W. Leigh (2002,2005). Cochlear Implants in Children: Ethics and Choices. Washington, DC: Gallaudet University Press.
- Cooper, Huw R. and Craddock, Louise C. (2006)Cochlear Implants A Practical Guide. London and Philadelphia: Whurr Publishers.
- Djourno A, Eyriès C. (1957). 'Prothèse auditive par excitation électrique à distance du nerf sensoriel à l'aide d'un bobinage inclus à demeure.' In: La Presse Médicale 65 no.63. 1957.
- Djourno A, Eyriès C, (1957) 'Vallencien B. De l'excitation électrique du nerf cochléaire chez l'homme, par induction à distance, à l'aide d'un micro-bobinage inclus à demeure.' CR de la société.de biologie. 423-4. March 9, 1957.
- Eisen MD (2003), 'Djourno, Eyries, and the first implanted electrical neural stimulator to restore hearing.' in: Otology and Neurotology. 2003 May;24(3):500-6.
- Grodin, M. (1997). Ethical Issues in Cochlear Implant Surgery: An Exploration into Disease, Disability, and the Best Interests of the Child. Kennedy Institute of Ethics Journal 7:231-251.
- Johnston, Trevor. (2004). W(h)ither the deaf Community? In 'American Annals of the deaf' (volume 148 no. 5),
- Lane, H. and Bahan, B. (1998). Effects of Cochlear Implantation in Young Children: A Review and a Reply from a DEAF-WORLD Perspective. Otolaryngology: Head and Neck Surgery 119:297-308.
- Lane, Harlan (1993), Cochlear Implants:Their Cultural and Historical Meaning. In 'deaf History Unveiled', ed. J.Van Cleve, 272-291. Washington, D.C. Gallaudet University Press.
- Lane, Harlan (1994), The Cochlear Implant Controversy. World Federation of the deaf News 2 (3):22-28.
- Litovsky, Ruth Y., et al. (2006). "Bilateral Cochlear Implants in Children: Localization Acuity Measured with Minimum Audible Angle." Ear & Hearing, 2006; 27; 43-59.
- Miyamoto, R.T.,K.I.Kirk, S.L.Todd, A.M.Robbins, and M.J.Osberger. (1995). Speech Perception Skills of Children with Multichannel Cochlear Implants or Hearing Aids. Annals of Otology, Rhinology and Laryngology 105 (Suppl.):334-337
- Officiers, P.E., et. a. (2005). "International Consensus on bilateral cochlear implants and bimodal stimulation." Acta Oto-Laryngologica, 2005; 125; 918-919.
- Osberger M.J. and Kessler, D. (1995). Issues in Protocol Design for Cochlear Implant Trials in Children: The Clarion Pediatric Study. Annals of Otology, Rhinology and Laryngology 9 (Suppl.):337-339.
- Reefhuis J, et al. (2003) Risk of Bacterial Meningitis in Children with Cochlear Implants, USA 1997-2002. New England Journal of Medicine, 2003; 349:435-445.
- Spencer, Patricia Elizabeth and Marc Marschark. (2003). Cochlear Implants: Issues and Implications. In 'Oxford Handbook of deaf Studies, Language and Education', ed. Marc Marschark and Patricia Elizabeth Spencer, 434-450. Oxford: Oxford University Press, 2003.
- 3M Power Point Presentation on the Cochlear Implant.
- Barton G. Kids Hear Now Cochlear Implant Family Resource Center, University of Miami School of Medicine
External links
- Cochlear Implants at the Open Directory Project
- Cochlear Implants Information from the National Institutes of Health (NIH).
- NASA Spinoff article on engineer Adam Kissiah's contribution to cochlear implants beginning in the 1970s.
- NPR Story about improvements to improve the processing of music. Includes simulations of what someone with implants might hear.
- Tuning In PBS article about advances in cochlear implant technology with simulations of what someone with each type of implant would hear.
- My Bionic Quest for Boléro (Wired, November 2005): Author Michael Chorost writes about his own implant and trying the latest software from researchers in a quest to hear music better.
Categories:- Australian inventions
- Artificial organs
- Otology
- Neuroprosthetics
- Implants
- NASA technology spinoffs
- Audiology
Wikimedia Foundation. 2010.