- Dentofacial osteotomy
-
A Dentofacial Osteotomy (also known as corrective jaw surgery) is an oral surgery where bone is cut, moved, modified, and realigned to correct a dentofacial deformity. The word “osteotomy” means the division, or excision of bone. The dental osteotomy allows surgeons to visualize the jawbone, and work accordingly.
The operation is used to correct jaw problems and dentofacial deformities like maxillary prognathisms, mandibular prognathisms, open bites, difficulty chewing, difficulty swallowing, temporomandibular joint disorder pains, excessive wear of the teeth, and receding chins. Many surgeons prefer this procedure for the correction of a dentofacial deformity due to its effectiveness.
Contents
History of the Dental Osteotomy
Mandible and maxilla osteotomies date to the 1940’s. They were used to correct dentofacial deformities like a malocclusion, and a prognathism.[1] Advances have been made in the procedures, and in the anesthesia used. In 1985, mandible and maxilla osteotomies were effectively used to correct more extreme deformities like receding chins, and to relieve pain from temporomandibular joint disorder (TMJ).
Prior to 1991, some patients undergoing a dentofacial osteotomy still had third molars (wisdom teeth), and had them removed during surgery. An extensive study done, by Dr. M Lacy and Dr. R Colcleugh, was used to identify threats of combining the two surgeries used 83 patients from the time span of 1987 and 1991. Patients were reviewed, and divided into two groups; those who had, and those who didn’t have their third molars extracted during the dentofacial Osteotomy. The study showed that 73% of patients developed an infection of the hardware inserted into the jaw when having their third molars removed during an osteotomy. The data indicated that getting the osteotomy and the third molar extraction at the same time highly increases the chances of infection development.[2]
Advances in the surgical techniques allow surgeons to perform the surgery under local anesthesia with assistance from intravenous sedation. Dr. Raffaini introduced this technique in 2002 after a four-year study done with local anesthesia and assistance from intravenous sedation. Prior to this, surgeons would fully sedate patients, hospitalizing them shortly after the surgery for a 2-3 day recovery, specifically from the anesthesia. Advancements allow surgeons to expand the use of an osteotomy on more parts of the jaws with faster recovery time, less pain, and no hospitalization; making the surgery more effective in respect to time and recovery.[3]
The procedure, which is strictly used for a mandibular (jaw) deformity and mobilization, has advanced from similar very effective procedures performed since 1985. The original mandible and maxilla osteotomy procedure still remains almost unchanged since it’s the simplest and still most effective for dentofacial deformity correction.
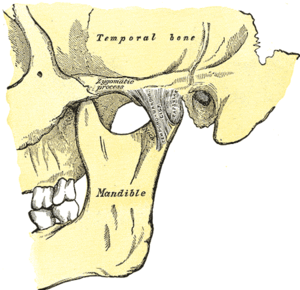
Diagnostics
A disproportionately grown upper or lower jaw causes dentofacial deformities. Chewing becomes problematic, and may also cause pain due to straining of the jaw muscle and bone. Deformities range from micrognathia, which is when the mandible doesn’t grow far forward enough (over bite), and when the mandible grows too much, causing an under bite; all of which are uncomfortable. Also, a total maxilla osteotomy is used to treat the “long face syndrome,” known as the skeptical open bite, idiopathic long face, hyper divergent face, total maxillary alveolar hyperplasia, and vertical maxillary excess. Prior to surgery, surgeons should take x-rays of the patient’s jaw to determine the deformity, and to make a plan of procedures.[4] Mandible osteotomies, or corrective jaw surgeries, benefit individuals who suffer from difficulty chewing, swallowing, TMJ pains, excessive wear of the teeth, open bites, overbites, underbites, or a receding chin.[5] The deformities listed above can be perfected by an osteotomy surgery of either the maxilla or mandible (whichever the deformity calls for), which is performed by an oral surgeon who is specialized in the working with both the upper and lower jaws.[6]
Procedures
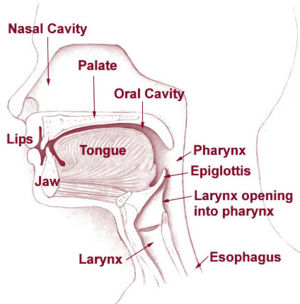
All dentofacial osteotomies are performed under general anesthesia, causing total unconsciousness. General anesthesia allows surgeons to perform dentofacial osteotomies effectively without involuntary muscle movement or complaints about minor pain. Prior to any Osteotomy, third molars (wisdom teeth) should be extracted to reduce the chance of infection. Every dentofacial osteotomy is performed using oscillating and reciprocating saws. Reciprocating saws are straight and are used for making straight bone cuts. Oscillating saws are angled, to different degrees, in order to make deep curved cuts for certain osteotomies like mandible angle reduction.
Maxilla Osteotomy (Upper Jaw)
- This procedure is intended for patients with an upper jaw deformity, or with an open bite.
Operating on the upper jaw requires surgeons to make incisions below both eye sockets, making it a bilateral osteotomy, enabling the whole upper jaw, along with the roof of the mouth and upper teeth, to move as one unit. At this time, the upper jaw can be moved and aligned correctly in order to fit the upper teeth in place with the lower teeth. Then, the jaw is stabilized using titanium screws that will eventually be grown over by bone, permanently staying in the mouth.[7]
Mandible Osteotomy (Lower Jaw)
- The mandible osteotomy is intended for those with a receded mandible (lower jaw) or an open bite, which may cause difficulty chewing and jaw pain.
For this procedure cuts are made behind the molars, in between the first and second molars, and lengthwise, detaching the front of the jaw so the palate (including the teeth and all) can move as one unit. From here, the surgeon can smoothly slide the mandible into its new position. Stabilization screws are used to support the jaw until the healing process is done.[7]
Sagittal Split Osteotomy
- This procedure is used to correct mandible retrusion and mandibular prognathism (over and under bite).
First, a horizontal cut is made on the inner side of the ramus mandibulae, extending anterally to the anterior portion of the ascending ramus. The cut is then made inferiorly on the ascending ramus to the descending ramus, extending to the lateral border of the mandible in the area between the first and second molar. At this time, a vertical cut is made extending inferior to the body of the mandible, to the inferior border of the mandible. All cuts are made into the middle of the bone, where bone marrow is present. Then, a chisel is inserted into the pre existing cuts and tapped gently in all areas to split the mandible of the left and right side. From here, the mandible can be moved either forwards or backwards. If sliding backwards, the distal segment must be trimmed to provide room in order to slide the mandible backwards. Lastly, the jaw is stabilized using stabilizing screws that are inserted extra-orally. The jaw is then wired shut for approximately 4-5 weeks.[7]
Genioplasty Osteotomy (Intra-oral)
- This procedure is used for the advancement (movement forward) or retraction (movement backwards) of the chin.
First, incisions are made from the first bicuspid to the first bicuspid, exposing the mandible. Then, soft tissue of the mandible is detached from the bone; done by stripping attaching tissues. A horizontal incision is then made inferior to the first bicuspids, bilaterally, where bone cuts (osteotomies) are made vertically inferior, extending to the inferior border of the mandible, thereby detaching the bony segments of the mandible. The bony segments are stabilized with titanium plates; no fixation (binding of the jaw) necessary. If advancement is indicated for the chin, there are inert products available to implant onto the mandible, utilizing titanium screws, bypassing bone cuts.[7]
Rapid Palatal Expansion Osteotomy
- When a patient has a constricted (oval shape) maxilla, but normal mandible, many orthodontists request a rapid palatal expansion.
This consists of the surgeon making horizontal cuts on the lateral board of the maxilla, extending anterally to the inferior border of the nasal cavity. At this time, a chisel designed for the nasal septum is utilized to detach the maxilla from the cranial base. Then, a pterygoid chisel, which is a curved chisel, is used on the left and right side of the maxilla to detach the pterygoid palates. Care must be taken as to not injure the inferior palatine artery. Prior to the procedure, the orthodontist has an orthopedic appliance attached to the maxilla teeth, bilaterally, extending over the palate with an attachment so the surgeon may use a hex-like screw to place into the device to push from anterior to posterior to start spreading the bony segments.[7] The expansion of the maxilla may take up to 8 weeks with the surgeon advancing the expander hex lock, sideways (← →), once a week.
Recovery
All dentofacial osteotomies require an extensive healing time. After surgery, the jaw is fragile and sensitive, requiring two to three months for healing. If the jaw is fixated (bound shut by wire) then the patient must remain that way for approximately four weeks. However, the jaw will still requires two to three months for proper healing. Lastly, if screws were inserted in the jaw, bone will typically grow over them during the two to three month healing period. Patients also may not drive or operate vehicles or large machinery during the consumption of painkillers, which are typically taken for six to eight days after the surgery, depending on the pain experienced. Immediately after surgery, patients must adhere to certain infection preventing instructions such as daily cleaning, and the consumption of antibiotics. Cleaning of the mouth should always be done regardless of surgery to ensure healthy, strong teeth. Patients are able to return to work 2-3 days after the surgery, but must follow the specific rules for recovery for ~8 weeks.[8]
Risks
Common complications with osteotomies consist of nerve damage that must be identified and fixed. Diagnostics for nerve damage consist of: brush-stroke directional discrimination (BSD), touch detection threshold (TD), warm/cold (W/C) and sharp/blunt discrimination (S/B), electrophysiological tests (mental nerve blink reflex (BR), nerve conduction study (NCS), and cold (CDT) and warm (WDT) detection thresholds.[9] The inferior alveolar nerve, which is a branch of the mandibular nerve, must be identified during surgery and worked around carefully in order to minimize nerve damage. Recovery from the nerve damage typically occurs within 3 months after repair. Third molars should be extracted well in advance of the surgery to minimize possible bacterial infections.
The biggest potential threat of oral maxillofacial surgery is any bacterial infection such as ones that travel from the blood stream to the heart, which can ultimately result in death. The most important and effective way of minimizing threat of a bacterial infection is to prevent it at all costs with pre and post antibiotic treatments.[10]
References
- ^ Puricelli, Edela. "A new technique for mandibular osteotomy." Head & Face Medicine 3.15 (2007). Head & Face Medicine. 13 Mar. 2007. BioMed Central Ltd. 27 Feb. 2009 http://www.head-face-med.com
- ^ M, Lacey, and Colcleugh R. "Infected screws in patients treated by mandibular sagittal split osteotomy.” Journal of oral and Maxillofacial Surgery 53.1 (2009): 510-12.
- ^ Raffaini, Micro. "The sagittal mandibular osteotomy under local anesthesia and intravenous sedation:Four years of multicenter experience." Adult Orthod Orthognath Surgery. 14. 17 (2002): 267-71.
- ^ Arnet, Gary F., and Linda M. Basehore. "Dentofacial reconstruction." The American Journal of Nursing. 12. 84 (1984): 1488-490.
- ^ "Corrective Jaw Surgery." American Association of Oral and Maxillofacial Surgeons (AAOMS). 07 Mar. 2009 <http://www.aaoms.org/jaw_surgery.php>.
- ^ Bell, William H., William R. Proffit, and Raymond P. White Jr. Surgical Correction of Dental Deformities. Canada: W. B. Saunders co., 1980.
- ^ a b c d e Dr. Charles A. Loschiavo, Oral and Maxillofacial Surgeon. Personal. 2 April 2009.
- ^ Mandible (Lower Jaw) Osteotomy. 2007. British Association of Oral and Maxillofacial Surgeon (BAOMS). 29 Feb. 2009 http://www.baoms.org.uk
- ^ Teerijoki-oksa, T., S. K. Jaaskelainen, and H. Forssell. "Recovery of nerve injury after mandibular sagittal split osteotomy. Diagnostic value of clinical and electrophysiologic tests in the follow-up.” International Journal of Oral and Maxillofacial Surgery 33.2 (2004): 134-40.
- ^ Hall, Gunnar, Anders Heimdahl, and Carl E. Nord. "Bacteremia after Oral Surgery and Prophylaxis for Endocarditis." Clinical Infectious Diseases 1.28 (1999): 1-8.
Categories:- Oral and maxillofacial surgery
- Oral surgery
- Jaw surgery
Wikimedia Foundation. 2010.